Amanita phalloides

| Amanita phalloides | |
|---|---|
 | |
| In Piacenza, Italy | |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Fungi |
| Division: | Basidiomycota |
| Class: | Agaricomycetes |
| Order: | Agaricales |
| Family: | Amanitaceae |
| Genus: | Amanita |
| Species: | A. phalloides |
| Binomial name | |
| Amanita phalloides | |
| Amanita phalloides | |
|---|---|
| Gills on hymenium | |
| Cap is convex or flat | |
| Hymenium is free | |
| Stipe has a ring and volva | |
| Spore print is white | |
| Ecology is mycorrhizal | |
| Edibility is deadly | |
Amanita phalloides (/æməˈnaɪtə fəˈlɔɪdiːz/), commonly known as the death cap, is a deadly poisonous basidiomycete fungus and mushroom, one of many in the genus Amanita. Originating in Europe[1] but later introduced to other parts of the world since the late twentieth century,[2][3][4][5] A. phalloides forms ectomycorrhizas with various broadleaved trees. In some cases, the death cap has been introduced to new regions with the cultivation of non-native species of oak, chestnut, and pine. The large fruiting bodies (mushrooms) appear in summer and autumn; the caps are generally greenish in colour with a white stipe and gills. The cap colour is variable, including white forms, and is thus not a reliable identifier.
These toxic mushrooms resemble several edible species (most notably Caesar's mushroom and the straw mushroom) commonly consumed by humans, increasing the risk of accidental poisoning. Amatoxins, the class of toxins found in these mushrooms, are thermostable: they resist changes due to heat, so their toxic effects are not reduced by cooking.
Amanita phalloides is the most poisonous of all known mushrooms.[6][7][8] It is estimated that as little as half a mushroom contains enough toxin to kill an adult human.[9] It is also the deadliest mushroom worldwide, responsible for 90% of mushroom-related fatalities every year.[10] It has been involved in the majority of human deaths from mushroom poisoning,[11] possibly including Roman Emperor Claudius in AD 54 and Holy Roman Emperor Charles VI in 1740.[12] It has also been the subject of much research and many of its biologically active agents have been isolated. The principal toxic constituent is α-Amanitin, which causes liver and kidney failure.
Taxonomy
[edit]The death cap is named in Latin as such in the correspondence between the English physician Thomas Browne and Christopher Merrett.[13] Also, it was described by French botanist Sébastien Vaillant in 1727, who gave a succinct phrase name "Fungus phalloides, annulatus, sordide virescens, et patulus"—a recognizable name for the fungus today.[14] Though the scientific name phalloides means "phallus-shaped", it is unclear whether it is named for its resemblance to a literal phallus or the stinkhorn mushrooms Phallus. In 1821, Elias Magnus Fries described it as Agaricus phalloides, but included all white amanitas within its description.[15] Finally, in 1833, Johann Heinrich Friedrich Link settled on the name Amanita phalloides,[16] after Persoon had named it Amanita viridis 30 years earlier.[17][18] Although Louis Secretan's use of the name A. phalloides predates Link's, it has been rejected for nomenclatural purposes because Secretan's works did not use binomial nomenclature consistently;[19][20] some taxonomists have, however, disagreed with this opinion.[21][22]
Amanita phalloides is the type species of Amanita section Phalloideae, a group that contains all of the deadly poisonous Amanita species thus far identified. Most notable of these are the species known as destroying angels, namely A. virosa, A. bisporigera and A. ocreata, as well as the fool's mushroom (A. verna). The term "destroying angel" has been applied to A. phalloides at times, but "death cap" is by far the most common vernacular name used in English. Other common names also listed include "stinking amanita"[23] and "deadly amanita".[24]
A rarely appearing, all-white form was initially described A. phalloides f. alba by Max Britzelmayr,[25][26] though its status has been unclear. It is often found growing amid normally colored death caps. It has been described, in 2004, as a distinct variety and includes what was termed A. verna var. tarda.[27] The true A. verna fruits in spring and turns yellow with KOH solution, whereas A. phalloides never does.[28]
Description
[edit]The death cap has a large and imposing epigeous (aboveground) fruiting body (basidiocarp), usually with a pileus (cap) from 5 to 15 centimetres (2 to 5+7⁄8 inches) across, initially rounded and hemispherical, but flattening with age.[29] The color of the cap can be pale-green, yellowish-green, olive-green, bronze, or (in one form) white; it is often paler toward the margins, which can have darker streaks;[30] it is also often paler after rain. The cap surface is sticky when wet and easily peeled—a troublesome feature, as that is allegedly a feature of edible fungi.[31] The remains of the partial veil are seen as a skirtlike, floppy annulus usually about 1 to 1.5 cm (3⁄8 to 5⁄8 in) below the cap. The crowded white lamellae (gills) are free. The stipe is white with a scattering of grayish-olive scales and is 8 to 15 cm (3+1⁄8 to 5+7⁄8 in) long and 1 to 2 cm (3⁄8 to 3⁄4 in) thick, with a swollen, ragged, sac-like white volva (base).[29] As the volva, which may be hidden by leaf litter, is a distinctive and diagnostic feature, it is important to remove some debris to check for it.[32] Spores: 7-12 x 6-9 μm. Smooth, ellipsoid, amyloid.[33]
The smell has been described as initially faint and honey-sweet, but strengthening over time to become overpowering, sickly-sweet and objectionable.[34] Young specimens first emerge from the ground resembling a white egg covered by a universal veil, which then breaks, leaving the volva as a remnant. The spore print is white, a common feature of Amanita. The transparent spores are globular to egg-shaped, measure 8–10 μm (0.3–0.4 mil) long, and stain blue with iodine.[34] The gills, in contrast, stain pallid lilac or pink with concentrated sulfuric acid.[35][36]
Biochemistry
[edit]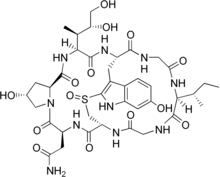

The species is now known to contain two main groups of toxins, both multicyclic (ring-shaped) peptides, spread throughout the mushroom tissue: the amatoxins and the phallotoxins. Another toxin is phallolysin, which has shown some hemolytic (red blood cell–destroying) activity in vitro. An unrelated compound, antamanide, has also been isolated.
Amatoxins consist of at least eight compounds with a similar structure, that of eight amino-acid rings; they were isolated in 1941 by Heinrich O. Wieland and Rudolf Hallermayer of the University of Munich.[2] Of the amatoxins, α-Amanitin is the chief component and along with β-amanitin is likely responsible for the toxic effects.[37][38] Their major toxic mechanism is the inhibition of RNA polymerase II, a vital enzyme in the synthesis of messenger RNA (mRNA), microRNA, and small nuclear RNA (snRNA). Without mRNA, essential protein synthesis and hence cell metabolism grind to a halt and the cell dies.[39] The liver is the principal organ affected, as it is the organ which is first encountered after absorption in the gastrointestinal tract, though other organs, especially the kidneys, are susceptible.[40] The RNA polymerase of Amanita phalloides is insensitive to the effects of amatoxins, so the mushroom does not poison itself.[41]
The phallotoxins consist of at least seven compounds, all of which have seven similar peptide rings. Phalloidin was isolated in 1937 by Feodor Lynen, Heinrich Wieland's student and son-in-law, and Ulrich Wieland of the University of Munich. Though phallotoxins are highly toxic to liver cells,[42] they have since been found to add little to the death cap's toxicity, as they are not absorbed through the gut.[39] Furthermore, phalloidin is also found in the edible (and sought-after) blusher (A. rubescens).[2] Another group of minor active peptides are the virotoxins, which consist of six similar monocyclic heptapeptides.[43] Like the phallotoxins, they do not induce any acute toxicity after ingestion in humans.[39]
The genome of the death cap has been sequenced.[44]
Similarity to edible species
[edit]A. phalloides is similar to the edible paddy straw mushroom (Volvariella volvacea)[45] and A. princeps, commonly known as "white Caesar".[46]
Some may mistake juvenile death caps for edible puffballs[47][48] or mature specimens for other edible Amanita species, such as A. lanei, so some authorities recommend avoiding the collecting of Amanita species for the table altogether.[49] The white form of A. phalloides may be mistaken for edible species of Agaricus, especially the young fruitbodies whose unexpanded caps conceal the telltale white gills; all mature species of Agaricus have dark-colored gills.[50]
In Europe, other similarly green-capped species collected by mushroom hunters include various green-hued brittlegills of the genus Russula and the formerly popular Tricholoma equestre, now regarded as hazardous owing to a series of restaurant poisonings in France. Brittlegills, such as Russula heterophylla, R. aeruginea, and R. virescens, can be distinguished by their brittle flesh and the lack of both volva and ring.[51] Other similar species include A. subjunquillea in eastern Asia and A. arocheae, which ranges from Andean Colombia north at least as far as central Mexico, both of which are also poisonous.
Distribution and habitat
[edit]The death cap is native to Europe, where it is widespread.[52] It is found from the southern coastal regions of Scandinavia in the north, to Ireland in the west, east to Poland and western Russia,[27] and south throughout the Balkans, in Greece, Italy, Spain, and Portugal in the Mediterranean basin, and in Morocco and Algeria in north Africa.[53] In west Asia, it has been reported from forests of northern Iran.[54] There are records from further east in Asia but these have yet to be confirmed as A. phalloides.[55]
By the end of the 19th century, Charles Horton Peck had reported A. phalloides in North America.[56] In 1918, samples from the eastern United States were identified as being a distinct though similar species, A. brunnescens, by George Francis Atkinson of Cornell University.[2] By the 1970s, it had become clear that A. phalloides does occur in the United States, apparently having been introduced from Europe alongside chestnuts, with populations on the West and East Coasts.[2][57] A 2006 historical review concluded the East Coast populations were inadvertently introduced, likely on the roots of other purposely imported plants such as chestnuts.[58] The origins of the West Coast populations remained unclear, due to scant historical records,[55] but a 2009 genetic study provided strong evidence for the introduced status of the fungus on the west coast of North America.[59] Observations of various collections of A. phalloides, from conifers rather than native forests, have led to the hypothesis that the species was introduced to North America multiple times. It is hypothesized that the various introductions led to multiple genotypes which are adapted to either oaks or conifers.[60]
A. phalloides were conveyed to new countries across the Southern Hemisphere with the importation of hardwoods and conifers in the late twentieth century. Introduced oaks appear to have been the vector to Australia and South America; populations under oaks have been recorded from Melbourne and Canberra[61][62][3] (where two people died in January 2012, of four who were poisoned)[63] and Adelaide,[64] as well as Uruguay.[65] It has been recorded under other introduced trees in Argentina.[4] Pine plantations are associated with the fungus in Tanzania[66] and South Africa, and it is also found under oaks and poplars in Chile.[67][68] A number of deaths in India have been attributed to it.[69]
Ecology
[edit]It is ectomycorrhizally associated with several tree species and is symbiotic with them. In Europe, these include hardwood and, less frequently, conifer species. It appears most commonly under oaks, but also under beeches, chestnuts, horse-chestnuts, birches, filberts, hornbeams, pines, and spruces.[25] In other areas, A. phalloides may also be associated with these trees or with only some species and not others. In coastal California, for example, A. phalloides is associated with coast live oak, but not with the various coastal pine species, such as Monterey pine.[70] In countries where it has been introduced, it has been restricted to those exotic trees with which it would associate in its natural range. There is, however, evidence of A. phalloides associating with hemlock and with genera of the Myrtaceae: Eucalyptus in Tanzania[66] and Algeria,[53] and Leptospermum and Kunzea in New Zealand,[25][71] suggesting that the species may have invasive potential.[55] It may have also been anthropogenically introduced to the island of Cyprus, where it has been documented to fruit within Corylus avellana plantations.[72]
Toxicity
[edit]
As the common name suggests, the fungus is highly toxic, and is responsible for the majority of fatal mushroom poisonings worldwide.[11][73] Its biochemistry has been researched intensively for decades,[2] and 30 grams (1.1 ounces), or half a cap, of this mushroom is estimated to be enough to kill a human.[74] On average, one person dies a year in North America from death cap ingestion.[46] The toxins of the death cap mushrooms primarily target the liver, but other organs, such as the kidneys, are also affected. Symptoms of death cap mushroom toxicity usually occur 6 to 12 hours after ingestion.[75] Symptoms of ingestion of the death cap mushroom may include nausea and vomiting, which is then followed by jaundice, seizures, and coma which will lead to death. The mortality rate of ingestion of the death cap mushroom is believed to be around 10–30%.[76]
Some authorities strongly advise against putting suspected death caps in the same basket with fungi collected for the table and to avoid even touching them.[31][77] Furthermore, the toxicity is not reduced by cooking, freezing, or drying.[78]
Poisoning incidents usually result from errors in identification. Recent cases highlight the issue of the similarity of A. phalloides to the edible paddy straw mushroom (Volvariella volvacea), with East- and Southeast-Asian immigrants in Australia and the West Coast of the U.S. falling victim. In an episode in Oregon, four members of a Korean family required liver transplants.[45] Many North American incidents of death cap poisoning have occurred among Laotian and Hmong immigrants, since it is easily confused with A. princeps ("white Caesar"), a popular mushroom in their native countries.[46] Of the 9 people poisoned in Australia's Canberra region between 1988 and 2011, three were from Laos and two were from China.[78] In January 2012, four people were accidentally poisoned when death caps (reportedly misidentified as straw mushrooms, which are popular in Chinese and other Asian dishes) were served for dinner in Canberra; all the victims required hospital treatment and two of them died, with a third requiring a liver transplant.[79]
Signs and symptoms
[edit]Death caps have been reported to taste pleasant.[2][80] This, coupled with the delay in the appearance of symptoms—during which time internal organs are being severely, sometimes irreparably, damaged—makes them particularly dangerous. Initially, symptoms are gastrointestinal in nature and include colicky abdominal pain, with watery diarrhea, nausea, and vomiting, which may lead to dehydration if left untreated, and, in severe cases, hypotension, tachycardia, hypoglycemia, and acid–base disturbances.[81][82] These first symptoms resolve two to three days after the ingestion. A more serious deterioration signifying liver involvement may then occur—jaundice, diarrhea, delirium, seizures, and coma due to fulminant liver failure and attendant hepatic encephalopathy caused by the accumulation of normally liver-removed substances in the blood.[23] Kidney failure (either secondary to severe hepatitis[43][83] or caused by direct toxic kidney damage[39]) and coagulopathy may appear during this stage. Life-threatening complications include increased intracranial pressure, intracranial bleeding, pancreatic inflammation, acute kidney failure, and cardiac arrest.[81][82] Death generally occurs six to sixteen days after the poisoning.[84]
It is noticed that after up to 24 hours have passed, the symptoms seem to disappear and the person might feel fine for up to 72 hours. Symptoms of liver and kidney damage start 3 to 6 days after the mushrooms were eaten, with the considerable increase of the transaminases.[85]
Mushroom poisoning is more common in Europe than in North America.[86] Up to the mid-20th century, the mortality rate was around 60–70%, but this has been greatly reduced with advances in medical care. A review of death cap poisoning throughout Europe from 1971 to 1980 found the overall mortality rate to be 22.4% (51.3% in children under ten and 16.5% in those older than ten).[87] This was revised to around 10–15% in surveys reviewed in 1995.[88]
Treatment
[edit]Consumption of the death cap is a medical emergency requiring hospitalization. The four main categories of therapy for poisoning are preliminary medical care, supportive measures, specific treatments, and liver transplantation.[89]
Preliminary care consists of gastric decontamination with either activated carbon or gastric lavage; due to the delay between ingestion and the first symptoms of poisoning, it is common for patients to arrive for treatment many hours after ingestion, potentially reducing the efficacy of these interventions.[89][90] Supportive measures are directed towards treating the dehydration which results from fluid loss during the gastrointestinal phase of intoxication and correction of metabolic acidosis, hypoglycemia, electrolyte imbalances, and impaired coagulation.[89]
No definitive antidote is available, but some specific treatments have been shown to improve survivability. High-dose continuous intravenous penicillin G has been reported to be of benefit, though the exact mechanism is unknown,[87] and trials with cephalosporins show promise.[91][92] Some evidence indicates intravenous silibinin, an extract from the blessed milk thistle (Silybum marianum), may be beneficial in reducing the effects of death cap poisoning. A long-term clinical trial of intravenous silibinin began in the US in 2010.[93] Silibinin prevents the uptake of amatoxins by liver cells, thereby protecting undamaged liver tissue; it also stimulates DNA-dependent RNA polymerases, leading to an increase in RNA synthesis.[94][95][96] According to one report[97] based on a treatment of 60 patients with silibinin, patients who started the drug within 96 hours of ingesting the mushroom and who still had intact kidney function all survived. As of February 2014 supporting research has not yet been published.
SLCO1B3 has been identified as the human hepatic uptake transporter for amatoxins; moreover, substrates and inhibitors of that protein—among others rifampicin, penicillin, silibinin, antamanide, paclitaxel, ciclosporin and prednisolone—may be useful for the treatment of human amatoxin poisoning.[98]
N-acetylcysteine has shown promise in combination with other therapies.[99] Animal studies indicate the amatoxins deplete hepatic glutathione;[100] N-acetylcysteine serves as a glutathione precursor and may therefore prevent reduced glutathione levels and subsequent liver damage.[101] None of the antidotes used have undergone prospective, randomized clinical trials, and only anecdotal support is available. Silibinin and N-acetylcysteine appear to be the therapies with the most potential benefit.[89] Repeated doses of activated carbon may be helpful by absorbing any toxins returned to the gastrointestinal tract following enterohepatic circulation.[102] Other methods of enhancing the elimination of the toxins have been trialed; techniques such as hemodialysis,[103] hemoperfusion,[104] plasmapheresis,[105] and peritoneal dialysis[106] have occasionally yielded success, but overall do not appear to improve outcome.[39]
In patients developing liver failure, a liver transplant is often the only option to prevent death. Liver transplants have become a well-established option in amatoxin poisoning.[81][82][107] This is a complicated issue, however, as transplants themselves may have significant complications and mortality; patients require long-term immunosuppression to maintain the transplant.[89] That being the case, the criteria have been reassessed, such as onset of symptoms, prothrombin time (PT), serum bilirubin, and presence of encephalopathy, for determining at what point a transplant becomes necessary for survival.[108][109][110] Evidence suggests, although survival rates have improved with modern medical treatment, in patients with moderate to severe poisoning, up to half of those who did recover suffered permanent liver damage.[111] A follow-up study has shown most survivors recover completely without any sequelae if treated within 36 hours of mushroom ingestion.[112]
Notable victims
[edit]Ce plat de champignons a changé la destinée de l'Europe.
[This mushroom dish has changed the destiny of Europe.]— Voltaire, Mémoires
Several historical figures may have died from A. phalloides poisoning (or other similar, toxic Amanita species). These were either accidental poisonings or assassination plots. Alleged victims of this kind of poisoning include Roman Emperor Claudius, Pope Clement VII, the Russian tsaritsa Natalia Naryshkina, and Holy Roman Emperor Charles VI.[12]
R. Gordon Wasson recounted[12] the details of these deaths, noting the likelihood of Amanita poisoning. In the case of Clement VII, the illness that led to his death lasted five months, making the case inconsistent with amatoxin poisoning. Natalya Naryshkina is said to have consumed a large quantity of pickled mushrooms prior to her death. It is unclear whether the mushrooms themselves were poisonous or if she succumbed to food poisoning.
Charles VI experienced indigestion after eating a dish of sautéed mushrooms. This led to an illness from which he died 10 days later—symptomatology consistent with amatoxin poisoning. His death led to the War of the Austrian Succession. Noted Voltaire, "this mushroom dish has changed the destiny of Europe."[12][113]
The case of Claudius's poisoning is more complex. Claudius was known to have been very fond of eating Caesar's mushroom. Following his death, many sources have attributed it to his being fed a meal of death caps instead of Caesar's mushrooms. Ancient authors, such as Tacitus and Suetonius, are unanimous about poison having been added to the mushroom dish, rather than the dish having been prepared from poisonous mushrooms. Wasson speculated the poison used to kill Claudius was derived from death caps, with a fatal dose of an unknown poison (possibly a variety of nightshade) being administered later during his illness.[12][114] Other historians have speculated that Claudius may have died of natural causes.
In July 2023, four people in Leongatha, Australia were taken to hospital after consuming a Beef Wellington suspected to have contained A. phalloides. Three of the four guests subsequently died, and one survived, later receiving a liver transplant. The woman who cooked the meal, Erin Patterson, was charged with murder in November 2023.[115]
See also
[edit]- List of Amanita species
- List of deadly fungi
- Hôpital Fernand-Widal – Paris hospital founded as Maison Dubois, known for expertise in treating mushroom poisoning
References
[edit]- ^ Cai, Qing; Tulloss, Rodham E; Tang, Li P; Tolgor, Bau; Zhang, Ping; Chen, Zuo H; Yang, Zhu L (21 June 2014). "Multi-locus phylogeny of lethal amanitas: Implications for species diversity and historical biogeography". BMC Evolutionary Biology. 14 (1): 143. Bibcode:2014BMCEE..14..143C. doi:10.1186/1471-2148-14-143. ISSN 1471-2148. PMC 4094918. PMID 24950598.
- ^ a b c d e f g Litten, W. (March 1975). "The most poisonous mushrooms". Scientific American. 232 (3): 90–101. Bibcode:1975SciAm.232c..90L. doi:10.1038/scientificamerican0375-90. PMID 1114308.
- ^ a b Cole, F.M. (June 1993). "Amanita phalloides in Victoria". Medical Journal of Australia. 158 (12): 849–850. doi:10.5694/j.1326-5377.1993.tb137675.x. PMID 8326898.
- ^ a b Hunzinker, A.T. (1983). "Amanita phalloides en las Sierras de Córdoba". Kurtziana (in Spanish). 16: 157–160. ISSN 0075-7314.
- ^ Pringle, Anne; Adams, Rachel I.; Cross, Hugh B.; Bruns, Thomas D. (18 February 2009). "The ectomycorrhizal fungus Amanita phalloides was introduced and is expanding its range on the west coast of North America". Molecular Ecology. 18 (5): 817–833. Bibcode:2009MolEc..18..817P. doi:10.1111/j.1365-294X.2008.04030.x. ISSN 0962-1083. PMID 19207260.
- ^ Rajarathnam, S.; Shashirekha, M.N. (2003), "MUSHROOMS AND TRUFFLES | Use of Wild Mushrooms", Encyclopedia of Food Sciences and Nutrition, Elsevier, pp. 4048–4054, doi:10.1016/b0-12-227055-x/00813-0, ISBN 978-0-12-227055-0, retrieved 3 June 2024
- ^ Madore, François; Bouchard, Josée (2019), "Plasmapheresis in Acute Intoxication and Poisoning", Critical Care Nephrology, Elsevier, pp. 595–600.e3, doi:10.1016/b978-0-323-44942-7.00100-x, ISBN 978-0-323-44942-7, retrieved 25 July 2024
- ^ Wiegand, Timothy J. (2024), "Mushrooms, cyclopeptide", Encyclopedia of Toxicology, Elsevier, pp. 549–553, doi:10.1016/b978-0-12-824315-2.01020-4, ISBN 978-0-323-85434-4, retrieved 3 June 2024
- ^ Madore, François; Bouchard, Josée (2019), "Plasmapheresis in Acute Intoxication and Poisoning", Critical Care Nephrology, Elsevier, pp. 595–600.e3, doi:10.1016/b978-0-323-44942-7.00100-x, ISBN 978-0-323-44942-7, retrieved 3 June 2024
- ^ Moor-Smith, Maxwell; Li, Raymond; Ahmad, Omar (2019). "The world's most poisonous mushroom, Amanita phalloides, is growing in BC". British Columbia Medical Journal. 61 (1) – via BMCJ.
- ^ a b Benjamin, p.200.
- ^ a b c d e Wasson, Robert Gordon (1972). "The death of Claudius, or mushrooms for murderers". Botanical Museum Leaflets, Harvard University. 23 (3): 101–128 (110). doi:10.5962/p.168556. ISSN 0006-8098. S2CID 87008723.
- ^ The "fungi Phalloides" I found not very far from Norwich, large and very fetid......I have a part of one dried still by me. Letter dated August 18th 1668 in Vol 3. The Works of Sir Thomas Browne ed. Simon Wilkins 1834
- ^ Vaillant, Sébastien (1727). Botanicon Parisiense (in Latin). Leide & Amsterdam: J. H. Verbeek and B. Lakeman. OCLC 5146641.
- ^ Fries, Elias Magnus (1821). Systema Mycologicum I (in Latin). Gryphiswaldiae: Ernesti Mauritii. OCLC 10717479.
- ^ (in German) Link JHF (1833) Grundriss der Kraeuterkunde IV. Haude und Spenerschen Buchhandlung (S.J. Joseephy), Berlin
- ^ Persoon, Christian Hendrik (1797). Tentamen Dispositionis Methodicae Fungorum (in Latin). Lipsiae: P.P. Wolf. OCLC 19300194.
- ^ Persoon, Christian Hendrik (1801). Synopsis Methodica Fungorum (in Latin). Göttingen: H. Dietrich. OCLC 28329773.
- ^ Donk, M.A. (June 1962). "On Secretan's Fungus Names". Taxon. 11 (5): 170–173. doi:10.2307/1216724. JSTOR 1216724.
- ^ Demoulin, V. (November 1974). "Invalidity of Names Published in Secretan's Mycographie Suisse and Some Remarks on the Problem of Publication by Reference". Taxon. 23 (5/6): 836–843. doi:10.2307/1218449. JSTOR 1218449. S2CID 88436479.
- ^ Singer, Rolf; Robert E. Machol (June 1962). "Are Secretan's Fungus Names Valid?". Taxon. 26 (2/3): 251–255. doi:10.2307/1220563. JSTOR 1220563.
- ^ Machol, Robert E. (August 1984). "Leave the Code Alone". Taxon. 33 (3): 532–533. doi:10.2307/1221006. JSTOR 1221006.
- ^ a b North, Pamela Mildred (1967). Poisonous plants and fungi in color. London: Blandford Press. OCLC 955264.
- ^ Benjamin, p.203
- ^ a b c Tulloss, Rodham E. "Amanita phalloidea". Studies in the Amanitaceae. Retrieved 22 May 2007.
- ^ Jordan & Wheeler, p. 109
- ^ a b Neville, Pierre; Poumarat, Serge (2004). Amaniteae: Amanita, Limacella and Torrendia. Fungi Europaei (9). Alassio: Edizioni Candusso. ISBN 978-88-901057-3-9.
- ^ Tulloss, Rodham E. "Amanita verna". Studies in the Amanitaceae. Retrieved 22 May 2007.
- ^ a b Bresinsky A, Besl H (1990). A Colour Atlas of Poisonous Fungi. Wolfe Publishing. pp. 26–9. ISBN 978-0-7234-1576-3.
- ^ Trudell, Steve; Ammirati, Joe (2009). Mushrooms of the Pacific Northwest. Timber Press Field Guides. Portland, OR: Timber Press. p. 87. ISBN 978-0-88192-935-5.
- ^ a b Jordan & Wheeler, p.99
- ^ Jordan & Wheeler, p.108
- ^ M., Kuo (May 2013). "Amanita phalloides (MushroomExpert.Com)". www.mushroomexpert.com. Retrieved 16 August 2023.
- ^ a b Zeitlmayr, p.61
- ^ Jordan, Michael (1995). The Encyclopedia of Fungi of Britain and Europe. David & Charles. p. 198. ISBN 978-0-7153-0129-6.
- ^ "California Fungi: Amanita phalloides". MykoWeb.com. Archived from the original on 1 June 2007. Retrieved 1 June 2007.
- ^ Köppel C (1993). "Clinical symptomatology and management of mushroom poisoning". Toxicon. 31 (12): 1513–40. Bibcode:1993Txcn...31.1513K. doi:10.1016/0041-0101(93)90337-I. PMID 8146866.
- ^ Dart, RC (2004). "Mushrooms". Medical toxicology. Philadelphia: Williams & Wilkins. pp. 1719–35. ISBN 978-0-7817-2845-4.
- ^ a b c d e Karlson-Stiber C, Persson H (2003). "Cytotoxic fungi — an overview". Toxicon. 42 (4): 339–49. Bibcode:2003Txcn...42..339K. doi:10.1016/S0041-0101(03)00238-1. PMID 14505933.
- ^ Benjamin, p.217
- ^ Horgen, Paul A.; Vaisius, Allan C.; Ammirati, Joseph F. (1978). "The insensitivity of mushroom nuclear RNA polymerase activity to inhibition by amatoxins". Archives of Microbiology. 118 (3): 317–9. Bibcode:1978ArMic.118..317H. doi:10.1007/BF00429124. PMID 567964. S2CID 37127957.
- ^ Wieland T, Govindan VM (1974). "Phallotoxins bind to actins". FEBS Lett. 46 (1): 351–3. Bibcode:1974FEBSL..46..351W. doi:10.1016/0014-5793(74)80404-7. PMID 4429639. S2CID 39255487.
- ^ a b Vetter, János (January 1998). "Toxins of Amanita phalloides". Toxicon. 36 (1): 13–24. Bibcode:1998Txcn...36...13V. doi:10.1016/S0041-0101(97)00074-3. PMID 9604278.
- ^ Pulman, Jane A.; Childs, Kevin L.; Sgambelluri, R. Michael; Walton, Jonathan D. (1 January 2016). "Expansion and diversification of the MSDIN family of cyclic peptide genes in the poisonous agarics Amanita phalloides and A. bisporigera". BMC Genomics. 17 (1): 1038. doi:10.1186/s12864-016-3378-7. ISSN 1471-2164. PMC 5159998. PMID 27978833.
- ^ a b Benjamin, pp.198–199
- ^ a b c Childs, Craig (1 February 2019). "Death-Cap Mushrooms Are Spreading Across North America". The Atlantic. Retrieved 5 February 2019.
- ^ Hall IR, Stephenson SE, Buchanan PK, Yn W, Cole AL (2003). Edible and poisonous mushrooms of the world. New Zealand Institute for Crop & Food Research Limited. pp. 131–3. ISBN 978-0-478-10835-4.
- ^ Friesen, M.S.; Pringle, A.; Callan, B.; Leather, A. (2005). "Amanita phalloides heads north". Conference Proceedings of the North American Congress of Clinical Toxicologists (Case Study).
- ^ Phillips, Roger (2005). Mushrooms and Other Fungi of North America. Buffalo: Firefly books. p. 14. ISBN 978-1-55407-115-9.
- ^ Heino, Lepp (9 October 2006). "Deathcap Mushroom: Amanita phalloides". Australian National Botanic Gardens. Archived from the original on 19 May 2007. Retrieved 12 June 2007.
- ^ Zeitlmayr, p.62
- ^ Lange, Lene (1974). "The distribution of macromycetes in Europe". Dansk Botanisk Arkiv. 30: 5–105. ISSN 0011-6211.
- ^ a b Malençon, Georges; R. Bertault (1970). Flore des Champignons Supérieurs du Maroc I. Travaux de l'Institut scientifique chérifien et de la Faculté des sciences. Série botanique et biologie végétale (32). Rabat: Faculté des Sciences. OCLC 915096.
- ^ Asef, M.R. 2009. Poisonous mushrooms of Iran. Iran-shenasi publishing.
- ^ a b c Pringle, Anne; Else C. Vellinga (July 2006). "Last chance to know? Using literature to explore the biogeography of and invasion biology of the death cap mushroom Amanita phalloides (Vaill. Ex Fr. :Fr) Link". Biological Invasions. 8 (5): 1131–1144. Bibcode:2006BiInv...8.1131P. doi:10.1007/s10530-005-3804-2. S2CID 5273858.
- ^ Peck, Charles H. (1897). Annual report of the state botanist. Albany: University of the State of New York. OCLC 1185748.
- ^ Benjamin, p.204
- ^ Berch, Shannon; Kroeger, Paul; Finston, Terrie (2016). "The Death Cap mushroom (Amanita phalloides) moves to a native tree in Victoria, British Columbia". Botany.
- ^ Pringle, Anne; Adams, Rachel I.; Cross, Hugh B.; Burns, Thomas D. (2009). "The ectomycorrhizal fungus Amanita phalloides was introduced and is expanding its range on the west coast of North America". Molecular Ecology. 18 (5): 817–833. Bibcode:2009MolEc..18..817P. doi:10.1111/j.1365-294X.2008.04030.x. PMID 19207260. S2CID 20554586.
- ^ Tanghe, L.J.; Simons, D.M. (1973). "Amanita phalloides in eastern United States". Mycologia. 65 (1): 99–108. doi:10.2307/3757790. JSTOR 3757790. PMID 4734427.
- ^ Westcott, Ben (18 March 2014). "Death cap mushroom in season; do not pick them". The Canberra Times. Fairfax Media. Archived from the original on 27 April 2014.
- ^ Reid, D.A. (1980). "A monograph of the Australian species of Amanita Pers. ex Hook (Fungi)". Australian Journal of Botany Supplementary Series. 8: 1–96.
- ^ Hall, Bianca (7 January 2012). "Death cap tragedy: bistro still closed". The Canberra Times. Fairfax Media. Archived from the original on 17 January 2012.
- ^ Death cap mushrooms growing in the hills Archived 18 June 2012 at the Wayback Machine Elisa Black, AdelaideNow.com.au, 7 January 2012, accessed 8 January 2012
- ^ Herter, W.G. (1934). "La aparición del hongo venenoso Amanita phalloides en Sudamérica". Revista Sudamericana de Botánica (in Spanish). 1: 111–119.
- ^ a b Pegler, D.N. (1977). A preliminary agaric flora of East Africa. Kew Bulletin Additional Series (6). London: Royal Botanic Gardens, Kew. ISBN 978-0-11-241101-7.
- ^ Valenzuella, E.; Moreno, G.; Jeria, M. (1992). "Amanita phalloides en bosques de Pinus radiata de la IX Region de Chile: taxonomia, toxinas, metodos de dedection, intoxicacion faloidiana". Boletín Micológico. 7: 17–21. ISSN 0716-114X.
- ^ Reid, D.A.; A. Eicker (1991). "South African fungi: the genus Amanita". Mycological Research. 95 (1): 80–95. doi:10.1016/S0953-7562(09)81364-6. ISSN 0953-7562.
- ^ Verma, N.; Bhalla, A.; Kumar, S.; Dhiman, R. K.; Chawla, Y. K. (2014). "Wild Mushroom Poisoning in North India: Case Series with Review of Literature". Journal of Clinical and Experimental Hepatology. 4 (4): 361–365. doi:10.1016/j.jceh.2014.09.004. PMC 4298634. PMID 25755582.
- ^ Arora, David (1986). Mushrooms demystified : a comprehensive guide to the fleshy fungi. Berkeley, California: Ten Speed Press. ISBN 978-0-89815-170-1.
- ^ Ridley, G.S. (1991). "The New Zealand Species of Amanita (Fungi: Agaricales)". Australian Systematic Botany. 4 (2): 325–354. doi:10.1071/SB9910325.
- ^ Loizides M, Bellanger JM, Yiangou Y, Moreau PA. (2018). Preliminary phylogenetic investigations into the genus Amanita (Agaricales) in Cyprus, with a review of previous records and poisoning incidents. Documents Mycologiques 37, 201–218.
- ^ Death Cap Mushroom Soup Claims Fourth Victim
- ^ Benjamin, p.211
- ^ Kent, D.R.; Willis, G. (1997). Poison Management Manual. British Columbia: The BC Drug and Poison Information Centre.
- ^ Garcia, J.; Costa, V.M.; Carvalho, A.; Baptista, P.; Guedes de Pinho, P.; de Lourdes Bastos, M.; Carvalho, F. (2015). "Amanita phalloides poisoning: Mechanisms of toxicity and treatment". Toxicology. 86: 41–55. doi:10.1016/j.fct.2015.09.008. hdl:10198/17717. PMID 26375431.
- ^ Carluccio A (2003). The Complete Mushroom Book. London: Quadrille. p. 224. ISBN 978-1-84400-040-1.
- ^ a b Trim Geoffrey M.; et al. (September 1999). "Poisoning by Amanita phalloides ("deathcap") mushrooms in the Australian Capital Territory". Medical Journal of Australia. 171 (5): 247–249. doi:10.5694/j.1326-5377.1999.tb123631.x. PMID 10495756. S2CID 39222950. Retrieved 22 May 2007.
- ^ Gardiner S (4 January 2012). "Two die after eating death cap mushrooms". Sydney Morning Herald. Fairfax Media. Retrieved 4 January 2012.
- ^ Cleland, John Burton (1976) [1934]. Toadstools and mushrooms and other larger fungi of South Australia. South Australian Government Printer. OCLC 15150059.
- ^ a b c Pinson CW, Daya MR, Benner KG, Norton RL, Deveney KE, Ascher NL, Roberts JP, Lake JR, Kurkchubasche AG, Ragsdale JW (May 1990). "Liver transplantation for severe Amanita phalloides mushroom poisoning". American Journal of Surgery. 159 (5): 493–9. doi:10.1016/S0002-9610(05)81254-1. PMID 2334013.
- ^ a b c Klein AS, Hart J, Brems JJ, Goldstein L, Lewin K, Busuttil RW (February 1989). "Amanita poisoning: treatment and the role of liver transplantation". American Journal of Medicine. 86 (2): 187–93. doi:10.1016/0002-9343(89)90267-2. PMID 2643869.
- ^ Nicholls DW, Hyne BE, Buchanan P (1995). "Death cap mushroom poisoning". The New Zealand Medical Journal. 108 (1001): 234. PMID 7603660.
- ^ Fineschi V, Di Paolo M, Centini F (1996). "Histological criteria for diagnosis of amanita phalloides poisoning". J. Forensic Sci. 41 (3): 429–32. doi:10.1520/JFS13929J. PMID 8656182.
- ^ "Death Cap Mushrooms". www.bccdc.ca. Retrieved 29 November 2023.
- ^ "Santa Cruz doctor helps save lives of family who ate poisonous mushrooms". Santa Cruz Sentinel. Archived from the original on 13 January 2012. Retrieved 6 January 2012.
- ^ a b Floerscheim, G.L.; O. Weber; P. Tschumi; M. Ulbrich; et al. (August 1982). "Die klinische knollenblatterpilzvergiftung (Amanita Phalloides): prognostische faktoren und therapeutische massnahmen (Clinical death-cap (Amanita phalloides) poisoning: prognostic factors and therapeutic measures.)". Schweizerische Medizinische Wochenschrift (in German). 112 (34): 1164–1177. PMID 6291147.
- ^ Benjamin, p.215
- ^ a b c d e Enjalbert F; Rapior S; Nouguier-Soulé J; Guillon S; Amouroux N; Cabot C (2002). "Treatment of amatoxin poisoning: 20-year retrospective analysis". Journal of Toxicology: Clinical Toxicology. 40 (6): 715–57. doi:10.1081/CLT-120014646. PMID 12475187. S2CID 22919515.
- ^ Vesconi S, Langer M, Iapichino G, Costantino D, Busi C, Fiume L (1985). "Therapy of cytotoxic mushroom intoxication". Critical Care Medicine. 13 (5): 402–6. doi:10.1097/00003246-198505000-00007. PMID 3987318. S2CID 23016936.
- ^ Benjamin, p.227
- ^ Neftel, K.; et al. (January 1988). "(Are cephalosporins more active than penicillin G in poisoning with the deadly Amanita?)". Schweizerische Medizinische Wochenschrift (in German). 118 (2): 49–51. PMID 3278370.
- ^ Gumz, Jomdi (10 May 2010). "Dominican doctors pioneering research on mushroom poisoning antidote". Santa Cruz Sentinel. Archived from the original on 26 January 2012. Retrieved 1 November 2010.
- ^ Hruby K, Csomos G, Fuhrmann M, Thaler H (1983). "Chemotherapy of Amanita phalloides poisoning with intravenous silibinin". Human Toxicology. 2 (2): 183–95. doi:10.1177/096032718300200203. PMID 6862461. S2CID 19805371.
- ^ Carducci, R.; et al. (May 1996). "Silibinin and acute poisoning with Amanita phalloides". Minerva Anestesiologica (in Italian). 62 (5): 187–93. PMID 8937042.
- ^ Jahn, W. (1980). "Pharmacokinetics of {3H}-methyl-dehydroxymethyl-amanitin in the isolated perfused rat liver, and the influence of several drugs". In Helmuth Faulstich, B. Kommerell & Theodore Wieland (ed.). Amanita toxins and poisoning. Baden-Baden: Witzstrock. pp. 80–85. ISBN 978-3-87921-132-6.
- ^ Adams, Cat (10 February 2014). "The Most Dangerous Mushroom Is Spreading. Here's How to Treat Poisoning". Slate.
- ^ Letschert K, Faulstich H, Keller D, Keppler D (May 2006). "Molecular characterization and inhibition of amanitin uptake into human hepatocytes". Toxicol. Sci. 91 (1): 140–49. doi:10.1093/toxsci/kfj141. PMID 16495352.
- ^ Montanini S, Sinardi D, Praticò C, Sinardi A, Trimarchi G (1999). "Use of acetylcysteine as the life-saving antidote in Amanita phalloides (death cap) poisoning. Case report on 11 patients". Arzneimittel-Forschung. 49 (12): 1044–47. doi:10.1055/s-0031-1300549. PMID 10635453. S2CID 40666108.
- ^ Kawaji A, Sone T, Natsuki R, Isobe M, Takabatake E, Yamaura Y (1990). "In vitro toxicity test of poisonous mushroom extracts with isolated rat hepatocytes". The Journal of Toxicological Sciences. 15 (3): 145–56. doi:10.2131/jts.15.145. PMID 2243367.
- ^ Chyka P, Butler A, Holliman B, Herman M (2000). "Utility of acetylcysteine in treating poisonings and adverse drug reactions". Drug Safety. 22 (2): 123–48. doi:10.2165/00002018-200022020-00005. PMID 10672895. S2CID 25061940.
- ^ Busi C, Fiume L, Costantino D, Langer M, Vesconi F (1979). "Amanita toxins in gastroduodenal fluid of patients poisoned by the mushroom, Amanita phalloides". New England Journal of Medicine. 300 (14): 800. doi:10.1056/NEJM197904053001418. PMID 423916.
- ^ Sabeel AI, Kurkus J, Lindholm T (1995). "Intensive hemodialysis and hemoperfusion treatment of Amanita mushroom poisoning". Mycopathologia. 131 (2): 107–14. doi:10.1007/BF01102888. PMID 8532053. S2CID 23001126.
- ^ Wauters JP, Rossel C, Farquet JJ (1978). "Amanita phalloides poisoning treated by early charcoal haemoperfusion". British Medical Journal. 2 (6150): 1465. doi:10.1136/bmj.2.6150.1465. PMC 1608737. PMID 719466.
- ^ Jander S, Bischoff J, Woodcock BG (2000). "Plasmapheresis in the treatment of Amanita phalloides poisoning: II. A review and recommendations". Therapeutic Apheresis. 4 (4): 308–12. doi:10.1046/j.1526-0968.2000.004004303.x. PMID 10975479.
- ^ Langer M, Vesconi S, Iapichino G, Costantino D, Radrizzani D (1980). "The early removal of amatoxins in the treatment of amanita phalloides poisoning". Klinische Wochenschrift (in German). 58 (3): 117–23. doi:10.1007/BF01477268. PMID 7366125. S2CID 39522161.
- ^ Ganzert M, Felgenhauer N, Zilker T (2005). "Indication of liver transplantation following amatoxin intoxication". Journal of Hepatology. 42 (2): 202–9. doi:10.1016/j.jhep.2004.10.023. PMID 15664245.
- ^ O'grady, John G.; Graeme J.M. Alexander; Karen M. Hayllar; Roger Williams; et al. (August 1989). "Early indicators of prognosis in fulminant hepatic failure". Gastroenterology. 97 (2): 439–445. doi:10.1016/0016-5085(89)90081-4. PMID 2490426.
- ^ Panaro, Fabrizio; Enzo Andorno; Nicola Morelli; Marco Casaccia; Giuliano Bottino; Ferruccio Ravazzoni; Monica Centanaro; Sara Ornis; Umberto Valente; et al. (April 2006). "Letter to the editor: Liver transplantation represents the optimal treatment for fulminant hepatic failure from Amanita phalloides poisoning". Transplant International. 19 (4): 344–5. doi:10.1111/j.1432-2277.2006.00275.x. PMID 16573553. S2CID 39474194.
- ^ Escudié L, Francoz C, Vinel JP, Moucari R, Cournot M, Paradis V, Sauvanet A, Belghiti J, Valla D, Bernuau J, Durand F (2007). "Amanita phalloides poisoning: reassessment of prognostic factors and indications for emergency liver transplantation". J. Hepatol. 46 (3): 466–73. doi:10.1016/j.jhep.2006.10.013. PMID 17188393.
- ^ Benjamin, pp.231–232
- ^ Giannini L, Vannacci A, Missanelli A, Mastroianni R, Mannaioni PF, Moroni F, Masini E (2007). "Amatoxin poisoning: A 15-year retrospective analysis and follow-up evaluation of 105 patients". Clinical Toxicology. 45 (5): 539–42. doi:10.1080/15563650701365834. PMID 17503263. S2CID 37788880.
- ^ Benjamin, p.35
- ^ Benjamin, pp.33–34
- ^ "Australia mushroom deaths: Memorial for couple draws hundreds". BBC. 31 August 2023.
Cited texts
[edit]- Benjamin, Denis R. (1995). Mushrooms: Poisons and Panaceas—A Handbook for Naturalists, Mycologists and Physicians. New York: WH Freeman and Company. ISBN 978-0-7167-2600-5.
- Jordan, Peter; Wheeler, Steven (2001). The Ultimate Mushroom Book. London: Hermes House. ISBN 978-1-85967-092-7.
- Zeitlmayr, Linus (1976). Wild Mushrooms: An Illustrated Handbook. Hertfordshire: Garden City Press. ISBN 978-0-584-10324-3.
External links
[edit]- UK Telegraph Newspaper (September 2008) - One woman dead, another critically ill after eating Death Cap fungi
- AmericanMushrooms.com - The Death Cap Mushroom Amanita phalloides
- Amanita phalloides: the death cap
- Amanita phalloides: Invasion of the Death Cap
- Key to species of Amanita Section Phalloideae from North and Central America - Amanita studies website
- California Fungi—Amanita phalloides
- Death cap in Australia - ANBG website
- On the Trail of the Death Cap Mushroom from National Public Radio
- "Amanita phalloides" at the Encyclopedia of Life




