HAVCR2

Hepatitis A virus cellular receptor 2 (HAVCR2), also known as T-cell immunoglobulin and mucin-domain containing-3 (TIM-3), is a protein that in humans is encoded by the HAVCR2 (TIM-3)gene. HAVCR2 was first described in 2002 as a cell surface molecule expressed on IFNγ producing CD4+ Th1 and CD8+ Tc1 cells.[5][6] Later, the expression was detected in Th17 cells,[7] regulatory T-cells,[8] and innate immune cells (dendritic cells, NK cells, monocytes, macrophages).[9][10] HAVCR2 receptor is a regulator of the immune response.
Discovery
[edit]In a screen to identify differentially expressed molecules between Th1 and Th2 cells, Vijay Kuchroo and colleagues first described HAVCR2/TIM-3 in 2002.[5] Kuchroo was the first to characterize the inhibitory function of TIM-3 and its role in inhibiting T cell responses in both autoimmunity and cancer.[11] Similar to other checkpoint inhibitors such as PD-1 and CTLA-4, TIM-3 has been successfully targeted to treat several solid and hematogenous malignancies, including melanoma, AML, and MDS.[12]
Classification
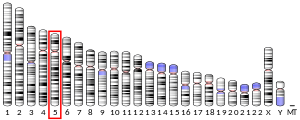
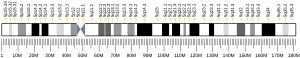
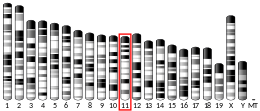
[edit]HAVCR2 /TIM-3 is member of TIM immunoregulatory proteins family which is encoded by gene on mouse chromosome 11B1.1 and on human chromosome 5q33.2. This chromosomal region has been repeatedly linked with asthma, allergy and autoimmunity. The TIM gene family include another eight members (TIM-1–8) on mouse chromosome and three members (TIM-1, TIM-3 and TIM-4) on human chromosome.[13][14][15]
Structure
[edit]HAVCR2 belongs to TIM family cell surface receptor proteins. These proteins share a similar structure, in which the extracellular region consists of membrane distal single variable immunoglobulin domain (IgV), a glycosylated mucin domain of variable length located closer to the membrane [16] transmembrane region, and intracellular stem. The IGV domain is form by two antiparallel beta sheets that are linked by disulfide bridges between four conserved cysteines. Cysteine bridges create a CC´ loop and an FG loop in the domain which make unique cleft characteristics for TIM-3 proteins. The cleft is stabilized by disulfide and hydrogen bonds and is a binding site for ligands such as CEACAM-1 and phosphatidylserine.[13][17] The extracellular portion of the IgV domain may also be glycosylated and this glycan-binding sites is recognizes by carbohydrate domain of another ligands galectin-9 (Gal-9).[13][17] The mucin domain is variable in a member of the TIM family, in TIM3 it is the smallest domain and has regions rich in serine, proline and threonine.[16][17] This region also contains target sites for O- and N-linked glycosylation. The transmembrane domain anchors the HAVCR2 protein in the cytoplasmic membrane of the cell.[14][16][18] The intracellular domain of HAVCR2 is called C-terminal cytoplasmic tail. It contains five conserved tyrosine residues that interact with multiple components of T-cell receptor (TCR) complex,[19][20] mediates intercellular signaling pathways and negatively regulates its function.[21]
Function
[edit]HAVCR2/TIM-3 is a transmembrane protein of T lymphocytes (CD4+ and CD8+ T cells), other lymphocytes (like NK cells), myeloid cells (monocytes, macrophages, DC, mast cells), or various cells in different tumor types.[9] The receptor is an immune checkpoint and together with other inhibitory receptors including programmed cell death protein 1 (PD-1) and lymphocyte activation gene 3 protein (LAG3) mediate the CD8+ T-cell exhaustion in terms of proliferation and secretion of cytokines such as TNF-alpha, IFN-gamma and IL-2.[22][23] Combined blockade of HAVCR2 and PD-1 led to improved CD8+ T-cell response during the lymphocytic choriomeningitis virus infection.[23] HAVCR2 and PD-1 may be responsible for NK cell exhaustion as well.[24] Similarly, HAVCR2/TIM-3 and VSIR/VISTA may co-exist on macrophages infiltrating different human and mouse tumours where they can co-regulate immunotherapy resistance.[9] HAVCR2 has also been shown as a CD4+ Th1-specific cell surface protein that regulates macrophage activation, regulates the production of cytokines and enhances the severity of experimental autoimmune encephalomyelitis in mice.[5] Is also known the free form of HAVCR2 outside the cell membrane (soluble form), lacking mucin and the transmembrane domain. However, the function of the soluble protein is unknown.[14]
Ligands
[edit]Gal-9
[edit]HAVCR2 is primarily activated by soluble galectin-9.[25] The engagement leads to stimulation of an influx of calcium to intracellular space and induction of programmed cell death, apoptosis, cell necrosis or T cell anergy.[26][17][18] As a consequence, a suppression of Th1 and Th17 responses and induction of immune tolerance occurs, gal-9/HAVCR2 increases the immunosuppressive activity of Treg cells.[14] In addition to galectin-9, several ligands have been identified, such as phosphatidylserine (PtdSer),[27] High Mobility Group Protein 1 (HMGB1)[28] and Carcinoembryonic Antigen Related Cell Adhesion Molecule 1 (CEACAM1).[14]
PtdSer
[edit]PtdSer is exposed on the surface of apoptotic cells and binds through the FG loop in the IgV domain. The binding of PtdSer with TIM-3 receptor has been shown to cause an uptake of apoptotic cells and is responsible for the cross-presentation of dying cell-associated antigens by dendritic cells.[29] PtdSer binds to the opposite side of the IgV domain of TIM-3 than Gal-9, and although this interaction of PtdSer to TIM-3 has five times less affinity than other members of the TIM family, Tim-3 can also bind some other ligand to phagocytose apoptotic cells.[14][29]
HMGB1
[edit]HMGB1 is alarmin and interacts with DNA released from dying cells or pathogen nucleid acid, facilitating absorption by cell and increasing nucleic acid sensing by endosomal Toll-like receptors (TLRs). HMGB1 binds to HAVCRS2/TIM3 on dendritic cells but its binding site has not been determined. TIM-3 receptor prevents the entry of the nucleic acids into the cell and suppresses activation of TLR signaling in dendritic cells.[14] So the binding of HMGB1suppresses activation of innate immune response.[28]
CEACAM1
[edit]The last known TIM3 receptor ligand is CEACAM1 glycoprotein. It is co-expressed with TIM3 T cells but also monocytes, macrophages, dendritic cells. It binds to the CC´ and FG loops of the TIM3 protein. CEACAM1 can also bind to TIM3 intracellularly (cis presentation) and is likely to be important for TIM-3 maturation on cell surface. The CEACAM1 binding contributes to the development of T cell tolerance, triggers the release of BAT3 from TIM-3 leading to inhibition of TCR signaling, and also inhibits the immune response of myeloid cells.[14]
Clinical significance
[edit]
HAVCR2 expression is up regulated in tumor-infiltrating lymphocytes in lung,[8] gastric,[30] head and neck cancer,[31] schwannoma,[32] melanoma[33] and follicular B-cell non-Hodgkin lymphoma.[34] It is also up-regulated in tumour-associated macrophages in various malignancies, including melanoma, especially in immunotherapy-resistant context.[9]
The HAVCR2 pathway may interact with the PD-1 pathway in the dysfunctional CD8+ T cells and Tregs in cancer.[35][8] HAVCR2 is mainly expressed on activated CD8+ T cells and suppresses macrophage activation following PD-1 inhibition.[36] Upregulation was observed in tumors progressing after anti-PD-1 therapy.[37] This seems to be a form of adaptive resistance to immunotherapy. Multiple phase 1/2 clinical trials with anti-HAVCR2 monoclonal antibodies (LY3321367,[38] Eli Lilly and Company; MBG453,[39] Novartis Pharmaceuticals; TSR-022,[40] Tesaro, Inc.) in combination with anti-PD-1 or anti-PD-L1 therapies are ongoing.
HAVCR2 is also an exhaustion maker for NK cells. Blockade of this receptor can improve the NK cells antitumor activity in esophageal cancer, melanoma and lung adenocarcinoma.[24]
The role of HAVCR2 in the T-cell dysfunction has been investigated in chronic viral infections. Together with PD-1, HAVCR2 negatively regulate CD8+ T-cells and thus, in vivo blockade of HAVCR2 and PD-1 led to the restoring of antiviral immunity.[41]
A recent genome-wide association study (GWAS) has found that genetic variations in HAVCR2 are associated with late-onset sporadic Alzheimer's disease (LOAD). HARVC2 is capable of interacting with amyloid-β precursor protein.[42]
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000135077 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000020399 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b c Monney L, Sabatos CA, Gaglia JL, Ryu A, Waldner H, Chernova T, et al. (January 2002). "Th1-specific cell surface protein Tim-3 regulates macrophage activation and severity of an autoimmune disease". Nature. 415 (6871): 536–541. doi:10.1038/415536a. PMID 11823861. S2CID 4403803.
- ^ "Entrez Gene: HAVCR2 hepatitis A virus cellular receptor 2".
- ^ Hastings WD, Anderson DE, Kassam N, Koguchi K, Greenfield EA, Kent SC, et al. (September 2009). "TIM-3 is expressed on activated human CD4+ T cells and regulates Th1 and Th17 cytokines". European Journal of Immunology. 39 (9): 2492–2501. doi:10.1002/eji.200939274. PMC 2759376. PMID 19676072.
- ^ a b c Gao X, Zhu Y, Li G, Huang H, Zhang G, Wang F, et al. (2012). "TIM-3 expression characterizes regulatory T cells in tumor tissues and is associated with lung cancer progression". PLOS ONE. 7 (2): e30676. Bibcode:2012PLoSO...730676G. doi:10.1371/journal.pone.0030676. PMC 3281852. PMID 22363469.
- ^ a b c d Vanmeerbeek I, Naulaerts S, Sprooten J, Laureano RS, Govaerts J, Trotta R, et al. (July 2024). "Targeting conserved TIM3+VISTA+ tumor-associated macrophages overcomes resistance to cancer immunotherapy". Science Advances. 10 (29): eadm8660. doi:10.1126/sciadv.adm8660. PMC 11259173. PMID 39028818.
- ^ Gleason MK, Lenvik TR, McCullar V, Felices M, O'Brien MS, Cooley SA, et al. (March 2012). "Tim-3 is an inducible human natural killer cell receptor that enhances interferon gamma production in response to galectin-9". Blood. 119 (13): 3064–3072. doi:10.1182/blood-2011-06-360321. PMC 3321868. PMID 22323453.
- ^ Kuchroo VK, Meyers JH, Umetsu DT, DeKruyff RH (April 2006). "TIM family of genes in immunity and tolerance". Advances in Immunology. 91 (1): 227–249. doi:10.1016/S0065-2776(06)91006-2. ISBN 9780120224913. PMID 16938542.
- ^ Rezaei M, Tan J, Zeng C, Li Y, Ganjalikhani-Hakemi M (2021). "TIM-3 in Leukemia; Immune Response and Beyond". Frontiers in Oncology. 11: 753677. doi:10.3389/fonc.2021.753677. PMC 8514831. PMID 34660319.
- ^ a b c Rodriguez-Manzanet R, DeKruyff R, Kuchroo VK, Umetsu DT (May 2009). "The costimulatory role of TIM molecules". Immunological Reviews. 229 (1): 259–270. doi:10.1111/j.1600-065x.2009.00772.x. PMC 3217781. PMID 19426227.
- ^ a b c d e f g h Wolf Y, Anderson AC, Kuchroo VK (March 2020). "TIM3 comes of age as an inhibitory receptor". Nature Reviews. Immunology. 20 (3): 173–185. doi:10.1038/s41577-019-0224-6. PMC 7327798. PMID 31676858.
- ^ Kuchroo VK, Dardalhon V, Xiao S, Anderson AC (August 2008). "New roles for TIM family members in immune regulation". Nature Reviews. Immunology. 8 (8): 577–580. doi:10.1038/nri2366. PMID 18617884. S2CID 31248.
- ^ a b c Cao E, Zang X, Ramagopal UA, Mukhopadhaya A, Fedorov A, Fedorov E, et al. (March 2007). "T cell immunoglobulin mucin-3 crystal structure reveals a galectin-9-independent ligand-binding surface". Immunity. 26 (3): 311–321. doi:10.1016/j.immuni.2007.01.016. PMID 17363302.
- ^ a b c d Ocaña-Guzman R, Torre-Bouscoulet L, Sada-Ovalle I (2016-06-13). "TIM-3 Regulates Distinct Functions in Macrophages". Frontiers in Immunology. 7: 229. doi:10.3389/fimmu.2016.00229. PMC 4904032. PMID 27379093.
- ^ a b Gorman JV, Colgan JD (August 2014). "Regulation of T cell responses by the receptor molecule Tim-3". Immunologic Research. 59 (1–3): 56–65. doi:10.1007/s12026-014-8524-1. PMC 4125508. PMID 24825777.
- ^ Lee J, Su EW, Zhu C, Hainline S, Phuah J, Moroco JA, et al. (October 2011). "Phosphotyrosine-dependent coupling of Tim-3 to T-cell receptor signaling pathways". Molecular and Cellular Biology. 31 (19): 3963–3974. doi:10.1128/MCB.05297-11. PMC 3187355. PMID 21807895.
- ^ van de Weyer PS, Muehlfeit M, Klose C, Bonventre JV, Walz G, Kuehn EW (December 2006). "A highly conserved tyrosine of Tim-3 is phosphorylated upon stimulation by its ligand galectin-9". Biochemical and Biophysical Research Communications. 351 (2): 571–576. doi:10.1016/j.bbrc.2006.10.079. PMID 17069754.
- ^ Tomkowicz B, Walsh E, Cotty A, Verona R, Sabins N, Kaplan F, et al. (2015). "TIM-3 Suppresses Anti-CD3/CD28-Induced TCR Activation and IL-2 Expression through the NFAT Signaling Pathway". PLOS ONE. 10 (10): e0140694. Bibcode:2015PLoSO..1040694T. doi:10.1371/journal.pone.0140694. PMC 4619610. PMID 26492563.
- ^ Blackburn SD, Shin H, Haining WN, Zou T, Workman CJ, Polley A, et al. (January 2009). "Coregulation of CD8+ T cell exhaustion by multiple inhibitory receptors during chronic viral infection". Nature Immunology. 10 (1): 29–37. doi:10.1038/ni.1679. PMC 2605166. PMID 19043418.
- ^ a b Jin HT, Anderson AC, Tan WG, West EE, Ha SJ, Araki K, et al. (August 2010). "Cooperation of Tim-3 and PD-1 in CD8 T-cell exhaustion during chronic viral infection". Proceedings of the National Academy of Sciences of the United States of America. 107 (33): 14733–14738. Bibcode:2010PNAS..10714733J. doi:10.1073/pnas.1009731107. PMC 2930455. PMID 20679213.
- ^ a b Zheng Y, Li Y, Lian J, Yang H, Li F, Zhao S, et al. (May 2019). "TNF-α-induced Tim-3 expression marks the dysfunction of infiltrating natural killer cells in human esophageal cancer". Journal of Translational Medicine. 17 (1): 165. doi:10.1186/s12967-019-1917-0. PMC 6528366. PMID 31109341.
- ^ Wada J, Kanwar YS (February 1997). "Identification and characterization of galectin-9, a novel beta-galactoside-binding mammalian lectin". The Journal of Biological Chemistry. 272 (9): 6078–6086. doi:10.1074/jbc.272.9.6078. PMID 9038233.
- ^ Zhu C, Anderson AC, Schubart A, Xiong H, Imitola J, Khoury SJ, et al. (December 2005). "The Tim-3 ligand galectin-9 negatively regulates T helper type 1 immunity". Nature Immunology. 6 (12): 1245–1252. doi:10.1038/ni1271. PMID 16286920. S2CID 24886582.
- ^ DeKruyff RH, Bu X, Ballesteros A, Santiago C, Chim YL, Lee HH, et al. (February 2010). "T cell/transmembrane, Ig, and mucin-3 allelic variants differentially recognize phosphatidylserine and mediate phagocytosis of apoptotic cells". Journal of Immunology. 184 (4): 1918–1930. doi:10.4049/jimmunol.0903059. PMC 3128800. PMID 20083673.
- ^ a b Chiba S, Baghdadi M, Akiba H, Yoshiyama H, Kinoshita I, Dosaka-Akita H, et al. (September 2012). "Tumor-infiltrating DCs suppress nucleic acid-mediated innate immune responses through interactions between the receptor TIM-3 and the alarmin HMGB1". Nature Immunology. 13 (9): 832–842. doi:10.1038/ni.2376. PMC 3622453. PMID 22842346.
- ^ a b Nakayama M, Akiba H, Takeda K, Kojima Y, Hashiguchi M, Azuma M, et al. (April 2009). "Tim-3 mediates phagocytosis of apoptotic cells and cross-presentation". Blood. 113 (16): 3821–3830. doi:10.1182/blood-2008-10-185884. PMID 19224762. S2CID 2539786.
- ^ Lu X, Yang L, Yao D, Wu X, Li J, Liu X, et al. (March 2017). "Tumor antigen-specific CD8+ T cells are negatively regulated by PD-1 and Tim-3 in human gastric cancer". Cellular Immunology. 313: 43–51. doi:10.1016/j.cellimm.2017.01.001. PMID 28110884.
- ^ Shayan G, Srivastava R, Li J, Schmitt N, Kane LP, Ferris RL (2017). "Adaptive resistance to anti-PD1 therapy by Tim-3 upregulation is mediated by the PI3K-Akt pathway in head and neck cancer". Oncoimmunology. 6 (1): e1261779. doi:10.1080/2162402X.2016.1261779. PMC 5283618. PMID 28197389.
- ^ Li Z, Liu X, Guo R, Wang P (May 2017). "TIM-3 plays a more important role than PD-1 in the functional impairments of cytotoxic T cells of malignant Schwannomas". Tumour Biology. 39 (5): 1010428317698352. doi:10.1177/1010428317698352. PMID 28475007.
- ^ Fourcade J, Sun Z, Benallaoua M, Guillaume P, Luescher IF, Sander C, et al. (September 2010). "Upregulation of Tim-3 and PD-1 expression is associated with tumor antigen-specific CD8+ T cell dysfunction in melanoma patients". The Journal of Experimental Medicine. 207 (10): 2175–2186. doi:10.1084/jem.20100637. PMC 2947081. PMID 20819923.
- ^ Yang ZZ, Grote DM, Ziesmer SC, Niki T, Hirashima M, Novak AJ, et al. (April 2012). "IL-12 upregulates TIM-3 expression and induces T cell exhaustion in patients with follicular B cell non-Hodgkin lymphoma". The Journal of Clinical Investigation. 122 (4): 1271–1282. doi:10.1172/JCI59806. PMC 3314462. PMID 22426209.
- ^ Anderson AC (May 2014). "Tim-3: an emerging target in the cancer immunotherapy landscape". Cancer Immunology Research. 2 (5): 393–398. doi:10.1158/2326-6066.CIR-14-0039. PMID 24795351. S2CID 20347477.
- ^ Dempke WC, Fenchel K, Uciechowski P, Dale SP (March 2017). "Second- and third-generation drugs for immuno-oncology treatment-The more the better?". European Journal of Cancer. 74: 55–72. doi:10.1016/j.ejca.2017.01.001. PMID 28335888.
- ^ Koyama S, Akbay EA, Li YY, Herter-Sprie GS, Buczkowski KA, Richards WG, et al. (February 2016). "Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints". Nature Communications. 7: 10501. Bibcode:2016NatCo...710501K. doi:10.1038/ncomms10501. PMC 4757784. PMID 26883990.
- ^ Clinical trial number NCT03099109 for "A Study of LY3321367 Alone or With LY3300054 in Participants With Advanced Relapsed/Refractory Solid Tumors" at ClinicalTrials.gov
- ^ Clinical trial number NCT02608268 for "Safety and Efficacy of MBG453 as Single Agent and in Combination With PDR001 in Patients With Advanced Malignancies" at ClinicalTrials.gov
- ^ Clinical trial number NCT02817633 for "Study of TSR-022, an Anti-TIM-3 Monoclonal Antibody, in Patients With Advanced Solid Tumors" at ClinicalTrials.gov
- ^ Jin HT, Anderson AC, Tan WG, West EE, Ha SJ, Araki K, et al. (August 2010). "Cooperation of Tim-3 and PD-1 in CD8 T-cell exhaustion during chronic viral infection". Proceedings of the National Academy of Sciences of the United States of America. 107 (33): 14733–14738. Bibcode:2010PNAS..10714733J. doi:10.1073/pnas.1009731107. PMC 2930455. PMID 20679213.
- ^ Wightman DP, Jansen IE, Savage JE, Shadrin AA, Bahrami S, Holland D, et al. (September 2021). "A genome-wide association study with 1,126,563 individuals identifies new risk loci for Alzheimer's disease". Nature Genetics. 53 (9): 1276–1282. doi:10.1038/s41588-021-00921-z. hdl:1871.1/61f01aa9-6dc7-4213-be2a-d3fe622db488. ISSN 1061-4036. PMC 10243600. PMID 34493870. S2CID 237442349.