Corpus luteum cyst
 From Wikipedia the free encyclopedia
From Wikipedia the free encyclopedia
| Corpus luteum cyst | |
|---|---|
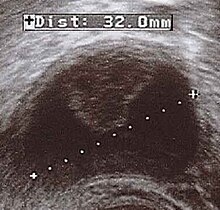 | |
| Corpus luteum cyst with bleeding. Fresh blood is anechoic (black). A protrusion of coagulated blood (lighter in color) can also be seen in the top of the cyst. | |
| Specialty | Gynaecology |
A corpus luteum cyst is a type of ovarian cyst which may rupture about the time of menstruation, and take up to three months to disappear entirely. A corpus luteum cyst rarely occurs in women over the age of 50, because eggs are no longer being released after menopause. Corpus luteum cysts may contain blood and other fluids. The physical shape of a corpus luteum cyst may appear as an enlargement of the ovary itself, rather than a distinct mass -like growth on the surface of the ovary.
Signs and symptoms[edit]
Corpus luteum cysts are a normal part of the menstrual cycle. They can, however, grow to almost 10 cm (4 inches) in diameter and have the potential to bleed into themselves or twist the ovary, causing pelvic or abdominal pain. It is possible the cyst may rupture, causing internal bleeding and pain. This pain typically disappears within a few days of the rupture. If the corpus luteum becomes large it may cause ovarian torsion, where the ovary twists and blood flow is cut off. Ovarian torsion is rare and is accompanied by severe pain.
Pathophysiology[edit]


This type of functional cyst occurs after an egg has been released from a follicle. The follicle then becomes a secretory gland that is known as the corpus luteum. The ruptured follicle begins producing large quantities of estrogen and progesterone in preparation for conception. If a pregnancy doesn't occur, the corpus luteum usually breaks down and disappears. It may, however, fill with fluid or blood, causing the corpus luteum to expand into a cyst, and stay in the ovary. Usually, this cyst is on only one side, and does not produce any symptoms.[1][2]
In women of reproductive age cysts with a diameter of less than 5 cm are common, clinically inconsequential, and almost always a physiological condition rather than a cancer or other disease condition.[3] In postmenopausal women the threshold for concern is 1 cm.[3] Although ovarian cancer may be cystic, it does not arise from benign corpus luteum cysts.[3] Medical specialty professional organizations recommend no follow-up imaging for cysts which are considered clinically inconsequential.[3]
A ruptured corpus luteum can cause hemoperitoneum with abdominal pain, and is a common condition in women of reproductive age. It may be confused with ectopic pregnancy.[4]
Interaction with medication[edit]
The fertility drug clomiphene citrate (Clomid, Serophene), used to induce ovulation, increases the risk of a corpus luteum cyst developing after ovulation. These cysts do not prevent or threaten a resulting pregnancy.[5][6] Women on birth control pills usually do not form these cysts; in fact, preventing these cysts is one way birth control pills work.[7] In contrast, the progesterone-only pill can cause increased frequency of these cysts.
References[edit]
- ^ "Ovarian Cysts: What You Need to Know about an Ovarian Cyst and PCOS".
- ^ "Corpus luteum cyst". Uni. Utah: Knowledge Weavers: Human Reproduction.
- ^ a b c d American College of Radiology, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American College of Radiology, archived from the original (PDF) on April 16, 2012, retrieved August 17, 2012, citing
- Levine, D.; Brown, D. L.; Andreotti, R. F.; Benacerraf, B.; Benson, C. B.; Brewster, W. R.; Coleman, B.; Depriest, P.; Doubilet, P. M.; Goldstein, S. R.; Hamper, U. M.; Hecht, J. L.; Horrow, M.; Hur, H. -C.; Marnach, M.; Patel, M. D.; Platt, L. D.; Puscheck, E.; Smith-Bindman, R. (2010). "Management of Asymptomatic Ovarian and Other Adnexal Cysts Imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement". Radiology. 256 (3): 943–954. doi:10.1148/radiol.10100213. PMC 6939954. PMID 20505067. S2CID 10270209.
- American College of Obstetricians and Gynecologists (2002). "ACOG Committee Opinion: Number 280, December 2002. The role of the generalist obstetrician-gynecologist in the early detection of ovarian cancer". Obstetrics and Gynecology. 100 (6): 1413–1416. doi:10.1016/S0029-7844(02)02630-3. PMID 12468197.
- American College of Obstetricians Gynecologists (2007). "ACOG Practice Bulletin No. 83: Management of Adnexal Masses". Obstetrics & Gynecology. 110 (1): 201–214. doi:10.1097/01.AOG.0000263913.92942.40. PMID 17601923.
- Timmerman, D.; Valentin, L.; Bourne, T. H.; Collins, W. P.; Verrelst, H.; Vergote, I.; International Ovarian Tumor Analysis (IOTA) Group (2000). "Terms, definitions and measurements to describe the sonographic features of adnexal tumors: A consensus opinion from the International Ovarian Tumor Analysis (IOTA) group". Ultrasound in Obstetrics and Gynecology. 16 (5): 500–505. doi:10.1046/j.1469-0705.2000.00287.x. PMID 11169340. S2CID 7553390.
- ^ Bauman, Renato; Horvat, Gordana (December 2018). "MANAGEMENT OF RUPTURED CORPUS LUTEUM WITH HEMOPERITONEUM IN EARLY PREGNANCY – A CASE REPORT". Acta Clinica Croatica. 57 (4): 785–788. doi:10.20471/acc.2018.57.04.24. PMC 6544092. PMID 31168219.
- ^ "Ovarian cysts: Causes". Mayo Clinic.
- ^ "Corpus luteum cyst". Mayo Clinic.
- ^ Hill DA. "Photos of the Ovaries". Women's Health Information. Archived from the original on March 21, 2007.