Pulmonary surfactant (medication)
 From Wikipedia the free encyclopedia
From Wikipedia the free encyclopedia
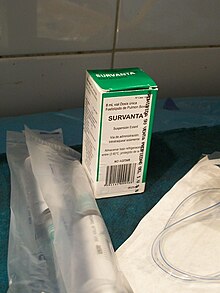 Beractant, surrounded by devices for its application. | |
| Clinical data | |
|---|---|
| Pronunciation | Curosurf, Survanta, others |
| Other names | Beractant, Poractant alfa, others |
| AHFS/Drugs.com | Monograph |
| License data | |
| ATC code | |
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
| UNII | |
Pulmonary surfactant is used as a medication to treat and prevent respiratory distress syndrome in newborn babies.[1]
Prevention is generally done in babies born at a gestational age of less than 32 weeks.[1] It is given by the endotracheal tube.[1] Onset of effects is rapid.[2] A number of doses may be needed.[2]
Side effects may include slow heart rate and low oxygen levels.[1] Its use is also linked with intracranial bleeding.[1] Pulmonary surfactant may be isolated from the lungs of cows or pigs or made artificially.[1][3][4]
Pulmonary surfactant was discovered in the 1950s and a manufactured version was approved for medical use in the United States in 1990.[3] It is on the World Health Organization's List of Essential Medicines.[5]
Medical uses
[edit]Pulmonary surfactant is used to treat and prevent respiratory distress syndrome in newborn babies.[1] Prevention is generally done in babies born less than 32 weeks gestational age.[1] Tentative evidence supports use in drowning.[6]
Surfactant administration can also be effective in meconium aspiration syndrome where it has been shown to help lower length of stay.[7][8]
For patients with acute respiratory distress syndrome (ARDS), surfactant has not been shown to reduce mortality. However, it may be beneficial in those with COVID-19 associated ARDS.[9][10]
Types
[edit]There are a number of types of pulmonary surfactants available. Like their natural counterparts, pulmonary surfactant preparations consist of phospholipids (mainly DPPC) combined with spreading agents such as SP-B and SP-C.[11] Ex-situ measurements of surface tension and interfacial rheology can help to understand the functionality of pulmonary surfactants.[12]
Synthetic pulmonary surfactants:
- Colfosceril palmitate (Exosurf) – a mixture of DPPC with hexadecanol and tyloxapol added as spreading agents
- Pumactant (Artificial Lung Expanding Compound or ALEC) – a mixture of DPPC and PG
- Lucinactant (KL4, trade name Surfaxin) – composed of DPPC, palmitoyl-oleoyl phosphatidylglycerol, and palmitic acid, combined with a 21 amino acid synthetic peptide (sinapultide) that mimics the C-terminal helical domain of SP-B.[13]
- Ventricute - DPPC, rSP-C
Animal-derived surfactants:
- Beractant (Survanta) – extracted from minced cow lung with additional DPPC, palmitic acid and tripalmitin, manufactured by Abbvie
- (Beraksurf) – extracted from minced cow lung with additional DPPC, palmitic acid and tripalmitin, manufactured by Tekzima
- Calfactant (Infasurf) – extracted from calf lung lavage fluid, manufactured by ONY Biotech.
- Poractant alfa (Curosurf) – extracted from material derived from minced pig lung
- Surfactant TA (Surfacten) – derived from cows, manufactured by Tokyo Tanabe Co. [14]
- Bovactant SF-RI (Alveofact) – extracted from cow lung lavage fluid, manufactured by Boehringer Ingelheim
History
[edit]Researcher John Clements identified surfactants and their role in the 1950s. Mary Ellen Avery soon after showed that the lungs of premature infants could not produce surfactants.[15]
Exosurf, Curosurf, Infasurf, and Survanta were the initial surfactants FDA approved for use in the U.S.[16]
In 2012, the US FDA approved an additional synthetic surfactant, lucinactant (Surfaxin).[17]
References
[edit]- ^ a b c d e f g h British National Formulary: BNF 69 (69 ed.). British Medical Association. 2015. p. 217. ISBN 9780857111562.
- ^ a b Martin RJ, Crowley MA (2013). "Respiratory Problems". In Fanaroff AA, Fanaroff JM (eds.). Klaus and Fanaroff's Care of the High-Risk Neonate, Expert Consult - Online and Print,6: Klaus and Fanaroff's Care of the High-Risk Neonate. Elsevier Health Sciences. p. 252. ISBN 978-1416040019. Archived from the original on 2017-01-09.
- ^ a b Lantos JD, Meadow WL (2006). "The Era of Exposed Ignorance, 1982-1992". Neonatal Bioethics: The Moral Challenges of Medical Innovation. JHU Press. pp. 54–56. ISBN 9780801883446. Archived from the original on 2017-01-09.
- ^ Wratney AT, Cheifetz IM (2006). "Gases and Drugs Used in Support of the Respiratory System". In Slonim AD, Pollack MM (eds.). Pediatric Critical Care Medicine. Lippincott Williams & Wilkins. pp. 724–725. ISBN 9780781794695. Archived from the original on 2017-01-09.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Ferguson JD, De Guzman J (2012). "Cardiac Arrest in Special Populations". In Brady B, Charlton NP, Lawner BJ, Sutherland SF (eds.). Cardiac Arrest, An Issue of Emergency Medicine Clinics. Elsevier Health Sciences. p. 175. ISBN 978-1455742769. Archived from the original on 2017-01-09.
- ^ El Shahed AI, Dargaville PA, Ohlsson A, Soll R (December 2014). "Surfactant for meconium aspiration syndrome in term and late preterm infants". The Cochrane Database of Systematic Reviews. 2014 (12): CD002054. doi:10.1002/14651858.CD002054.pub3. PMC 7027383. PMID 25504256.
- ^ Walsh B (2019). Neonatal and Pediatric Respiratory Care. Elsevier. pp. 244–261. ISBN 978-0-323-47947-9.
- ^ Davidson WJ, Dorscheid D, Spragg R, Schulzer M, Mak E, Ayas NT (2006). "Exogenous pulmonary surfactant for the treatment of adult patients with acute respiratory distress syndrome: results of a meta-analysis". Critical Care. 10 (2): R41. doi:10.1186/cc4851. PMC 1550886. PMID 16542488.
- ^ Heching M, Lev S, Shitenberg D, Dicker D, Kramer MR (July 2021). "Surfactant for the Treatment of ARDS in a Patient With COVID-19". Chest. 160 (1): e9–e12. doi:10.1016/j.chest.2021.01.028. PMC 7825915. PMID 33493441.
- ^ Nkadi PO, Merritt TA, Pillers DA (June 2009). "An overview of pulmonary surfactant in the neonate: genetics, metabolism, and the role of surfactant in health and disease". Molecular Genetics and Metabolism. 97 (2): 95–101. doi:10.1016/j.ymgme.2009.01.015. PMC 2880575. PMID 19299177.
- ^ Bertsch P, Bergfreund J, Windhab EJ, Fischer P (August 2021). "Physiological fluid interfaces: Functional microenvironments, drug delivery targets, and first line of defense". Acta Biomaterialia. 130: 32–53. doi:10.1016/j.actbio.2021.05.051. hdl:20.500.11850/498803. PMID 34077806. S2CID 235323337.
- ^ "KL4 Surfactant Technology". Windtree Therapeutics, Inc. Archived from the original on July 29, 2018. Retrieved 29 November 2017.
- ^ "T 0723/94 (Surfactant composition/TOKYO TANABE CO) of 18.2.1999". European Patent Office. Retrieved 2022-04-30.
- ^ Palca J (3 August 2015). "How A Scientist's Slick Discovery Helped Save Preemies' Lives". NPR. Archived from the original on 3 August 2015. Retrieved 3 August 2015.
- ^ Taeusch HW, Lu K, Ramierez-Schrempp D (2002). "Improving pulmonary surfactants" (PDF). Acta Pharmacologica Sinica. 23 Suppl: 11–5. Archived (PDF) from the original on 2015-03-01.
- ^ "Surfaxin (lucinactant) Intratracheal Suspension". Drug Approval Package. U.S. Food and Drug Administration. Retrieved 2022-04-30.
External links
[edit]- "Poractant alfa". Drug Information Portal. U.S. National Library of Medicine.
- "Beractant". Drug Information Portal. U.S. National Library of Medicine.
- "Calfactant". Drug Information Portal. U.S. National Library of Medicine.