Colorectal adenoma

| Colorectal adenoma | |
|---|---|
 | |
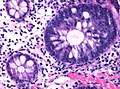
| Tubulovillous adenoma (tubular component – left of image, villous component – right of image). H&E stain. | |
| Specialty | Gastroenterology |
| Symptoms | Asymptomatic, rectal bleeding |
| Complications | Colorectal cancer |
| Diagnostic method | Colonoscopy |
| Treatment | Polypectomy |
The colorectal adenoma is a benign glandular tumor of the colon and the rectum. It is a precursor lesion of the colorectal adenocarcinoma (colon cancer).[1][2][3] They often manifest as colorectal polyps.
Comparison table
[edit]
| Type | Risk of containing malignant cells | Histopathology definition |
|---|---|---|
| Tubular adenoma | 2% at 1.5 cm[4] | Over 75% of volume has tubular appearance.[5] |
| Tubulovillous adenoma | 20% to 25%[6] | 25–75% villous[5] |
| Villous adenoma | 15%[7] to 40%[6] | Over 75% villous[5] |
| Sessile serrated adenoma (SSA)[8] |
|
Tubular adenoma
[edit]In contrast to hyperplastic polyps, these display dysplasia.[citation needed]
Tubulovillous adenoma
[edit]Tubulovillous adenoma, TVA are considered to have a higher risk of becoming malignant (cancerous) than tubular adenomas.[9]
- Normal (left) versus dysplastic (large at right) colonic crypts, the latter conferring a diagnosis of a tubular and/or villous adenoma.
- Histopathology of high-grade dysplasia in a tubulovillous adenoma, in this case seen mainly as loss of cell polarity, as cells become more plump and haphazard than the elongated and parallel nuclei of surrounding low-grade dysplasia.
Villous adenoma
[edit]
These adenomas may become malignant (cancerous). Villous adenomas have been demonstrated to contain malignant portions in about 15–25% of cases, approaching 40% in those over 4 cm in diameter.[7] Colonic resection may be required for large lesions. These can also lead to secretory diarrhea with large volume liquid stools with few formed elements. They are commonly described as secreting large amounts of mucus, resulting in hypokalaemia in patients. On endoscopy, a "cauliflower' like mass is described due to villi stretching. Being an adenoma, the mass is covered in columnar epithelial cells.[citation needed]
Sessile serrated adenoma
[edit]
Sessile serrated adenomas are characterized by (1) basal dilation of the crypts, (2) basal crypt serration, (3) crypts that run horizontal to the basement membrane (horizontal crypts), and (4) crypt branching. The most common of these features is basal dilation of the crypts.
See also
[edit]References
[edit]- ^ Hardcastle, J. D.; Armitage, N. C. (1984). "Early diagnosis of colorectal cancer: A review". Journal of the Royal Society of Medicine. 77 (8): 673–6. doi:10.1177/014107688407700812. PMC 1440108. PMID 6384511.
- ^ Schofield, P. F.; Jones, D. J. (1992). "ABC of colorectal diseases. Colorectal neoplasia—I: Benign colonic tumours". BMJ (Clinical Research Ed.). 304 (6840): 1498–500. doi:10.1136/bmj.304.6840.1498. PMC 1882234. PMID 1319254.
- ^ Srivastava, S; Verma, M; Henson, D. E. (2001). "Biomarkers for early detection of colon cancer". Clinical Cancer Research. 7 (5): 1118–26. PMID 11350874.
- ^ Minhhuyen Nguyen. "Polyps of the Colon and Rectum". MSD Manual. Last full review/revision June 2019
- ^ a b c Bosman, F. T. (2010). WHO classification of tumours of the digestive system. Lyon: International Agency for Research on Cancer. ISBN 978-92-832-2432-7. OCLC 688585784.
- ^ a b Amersi, Farin; Agustin, Michelle; Ko, Clifford Y (2005). "Colorectal Cancer: Epidemiology, Risk Factors, and Health Services". Clinics in Colon and Rectal Surgery. 18 (3): 133–140. doi:10.1055/s-2005-916274. ISSN 1531-0043. PMC 2780097. PMID 20011296.
- ^ a b Alnoor Ramji. "Villous Adenoma Follow-up". Medscape. Updated: Oct 24, 2016
- ^ Rosty, C; Hewett, D. G.; Brown, I. S.; Leggett, B. A.; Whitehall, V. L. (2013). "Serrated polyps of the large intestine: Current understanding of diagnosis, pathogenesis, and clinical management". Journal of Gastroenterology. 48 (3): 287–302. doi:10.1007/s00535-012-0720-y. PMC 3698429. PMID 23208018.
- ^ Levine JS, Ahnen DJ (December 2006). "Clinical practice. Adenomatous polyps of the colon". N. Engl. J. Med. 355 (24): 2551–7. doi:10.1056/NEJMcp063038. PMID 17167138.