Isoprenaline

Isoprenaline, also known as isoproterenol and sold under the brand name Isuprel among others, is a sympathomimetic medication which is used in the treatment of acute bradycardia (slow heart rate), heart block, and rarely for asthma, among other indications.[9] It is used by injection into a vein, muscle, fat, or the heart, by inhalation, and in the past under the tongue or into the rectum.[3][4]
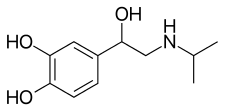
Side effects of isoprenaline include rapid heart beat, heart palpitations, and arrhythmias, among others.[9] Isoprenaline is a selective agonist of the β-adrenergic receptors, including both the β1- and β2-adrenergic receptors.[9] By activating these receptors, it increases heart rate and the force of heart contractions.[10] Chemically, isoprenaline is a synthetic catecholamine and is the N-isopropyl analogue of norepinephrine (noradrenaline) and epinephrine (adrenaline).[11][3][12][13]
Isoprenaline was one of the first synthetic sympathomimetic amines and was the first selective β-adrenergic receptor agonist.[7][14] The medication was discovered in 1940[5] and was introduced for medical use in 1947.[15]
Medical uses
[edit]Isoprenaline is used to treat heart block and episodes of Adams–Stokes syndrome that are not caused by ventricular tachycardia or fibrillation, in emergencies for cardiac arrest until electric shock can be administered, for bronchospasm occurring during anesthesia, and as an adjunct in the treatment of hypovolemic shock, septic shock, low cardiac output (hypoperfusion) states, congestive heart failure, and cardiogenic shock.[9] It is also used to prevent Torsades de Pointes in patients with long QT refractory to magnesium and to treat patients with intermittent Torsades de Pointes refractory to treatment with magnesium.[16] Isoprenaline is used in the acute management of bradycardia, though not in the chronic treatment of bradycardia.[17]
Historically, it was used to treat asthma via metered aerosol or nebulizing devices; it was also available in sublingual, oral, intravenous, and intramuscular formulations.[15] The U.S. National Asthma Education and Prevention Program Expert Panel recommends against its use as a nebulizer for acute bronchoconstriction.[18]
Available forms
[edit]Many formulations of isoprenaline appear to have been discontinued in the United States and many other countries.[4][1][2][3] In the United States, it remains available only as an injectable solution.[4] It was previously also available in the United States as a solution, metered aerosol, powder, or disc for inhalation and as a tablet for sublingual and rectal administration, but these formulations were discontinued.[4]
Contraindications
[edit]It should not be used in people with tachyarrhythmias (except in special circumstances),[19] tachycardia or heart block caused by digitalis poisoning, ventricular arrhythmias which require inotropic therapy, or with angina.[9]
Side effects
[edit]Side effects of isoprenaline may include nervousness, headache, dizziness, nausea, blurred vision, tachycardia, palpitations, angina, Adams-Stokes attacks, pulmonary edema, hypertension, hypotension, ventricular arrhythmias, tachyarrhythmias, difficulty breathing, sweating, mild tremors, weakness, flushing, and pallor.[9] Isoprenaline has been reported to cause insulin resistance leading to diabetic ketoacidosis.[20]
Overdose
[edit]Overdose of isoprenaline may produce effects including tachycardia, arrhythmias, palpitations, angina, hypotension, hypertension, and myocardial necrosis.[3][9]
Pharmacology
[edit]Pharmacodynamics
[edit]Isoprenaline is a β1- and β2-adrenergic receptor full agonist and has almost no activity at the α-adrenergic receptors at lower concentrations.[15][21] It has similar affinity for the β1- and β2-adrenergic receptors.[21][8] At higher concentrations, isoprenaline can also evoke responses mediated by α-adrenergic receptors.[8][22][23] Its agonist effects at the trace amine-associated receptor 1 (TAAR1) additionally provide it with pharmacodynamic effects that resemble those of the endogenous trace amines, like tyramine.[24]
Isoprenaline's effects on the cardiovascular system (non-selective) relate to its actions on cardiac β1-adrenergic receptors and β2-adrenergic receptors on smooth muscle within the tunica media of arterioles. Isoprenaline has positive inotropic and chronotropic effects on the heart. β2-Adrenergic receptor stimulation in arteriolar smooth muscle induces vasodilation. Its inotropic and chronotropic effects elevate systolic blood pressure, while its vasodilatory effects tend to lower diastolic blood pressure. The overall effect is to decrease mean arterial pressure due to the vasodilation caused by β2-adrenergic receptor activation.[25]
The isopropylamine group in isoprenaline makes it selective for β-adrenergic receptors.[26]
The adverse effects of isoprenaline are also related to the drug's cardiovascular effects. Isoprenaline can produce tachycardia (an elevated heart rate), which predisposes people who take it to cardiac arrhythmias.[15]
Pharmacokinetics
[edit]Absorption
[edit]Data on the absorption of isoprenaline are limited.[3] Oral isoprenaline is well-absorbed but is subject to strong first-pass metabolism[27] and is approximately 1,000 times less potent than intravenous administration.[6] Hence, its oral bioavailability is very low.[5][6] Another study suggested that its oral bioavailability, based on pharmacodynamic activity via different routes, was slightly less than 4%.[27][28]
Distribution
[edit]Isoprenaline is minimally able to cross the blood–brain barrier and hence is a peripherally selective drug.[29][30] This is attributed to its high hydrophilicity.[29] Whereas the extraction of isoprenaline in a single passage of the brain circulation following intravenous injection in humans was 3.8%, the extraction of propranolol, which is a more lipophilic compound and is readily able to cross into the brain, was 63.0%.[29]
The plasma protein binding of isoprenaline is 68.8 ± 1.2%.[3] It is bound mainly to albumin.[3]
Metabolism
[edit]Isoprenaline is metabolized by catechol O-methyltransferase (COMT) and conjugation by sulfation.[7][31][32][3] It does not appear to be glucuronidated.[7] There is very large interindividual variability in the sulfation of isoprenaline.[7] The free catechol hydroxyl groups keep it susceptible to enzymatic metabolism.[26] The drug is a poor substrate for monoamine oxidase (MAO) and is not metabolized by this enzyme.[7][9] This is in contrast to epinephrine and norepinephrine.[7] Isoprenaline is much more strongly metabolized and conjugated with oral administration than with intravenous administration.[6] Its metabolite 3-O-methylisoprenaline, formed by COMT, is active as a weak β-adrenergic receptor antagonist.[7]
Elimination
[edit]Isoprenaline is excreted primarily in the urine, as sulfate conjugates.[7][31][32][3] It is excreted 59 to 107% in urine and 12 to 27% in feces.[3] A majority of isoprenaline is excreted in urine in conjugated form, whereas 6.5 to 16.2% is excreted as unchanged isoprenaline and 2.6 to 11.4% is excreted as 3-O-methylisoprenaline and conjugates.[3][6]
The elimination half-life of isoprenaline by intravenous administration is approximately 2.5 to 5 minutes.[3] Its half-life with oral administration is approximately 40 minutes.[3][6]
Chemistry
[edit]Isoprenaline, also known as N-isopropyl-3,4,β-trihydroxyphenethylamine or as N-isopropylnorepinephrine, is a substituted phenethylamine and synthetic catecholamine derivative.[11][3][12][9] It is the N-isopropyl analogue of norepinephrine (3,4,β-trihydroxyphenethylamine) and epinephrine (3,4,β-trihydroxy-N-methylphenethylamine).[11][13]
Isoprenaline is a small-molecule compound with the molecular formula C11H17NO3 and a molecular weight of 211.26 g/mol.[11][3][12][9] It is a hydrophilic compound[29] with a predicted log P of -0.6 to 0.25.[11][3][12] For comparison, the experimental log P values of epinephrine and norepinephrine are -1.37 and -1.24, respectively.[33][34]
Isoprenaline is used pharmaceutically as the hydrochloride and sulfate salts.[1] It is also used to a much lesser extent as the free base.[1]
Isoprenaline is a racemic mixture of levorotatory and dextrorotatory enantiomers.[11][3][12] The levorotatory or (R)-enantiomer of isoprenaline is known as levisoprenaline (INN) but was never marketed.[35][36][37]
Synthetic analogues closely related to isoprenaline include arbutamine, dichloroisoprenaline (dichloroisoproterenol), hexoprenaline, isoetharine (α-ethylisoprenaline), orciprenaline (metaproterenol; a positional isomer of isoprenaline), prenalterol, and soterenol (3-methanesulfonamidylisoprenaline), among others.[5]
History
[edit]Isoprenaline was discovered in 1940[5] and was developed in the 1940s.[7] It was first approved for medical use in 1947 in the United States.[15] Isoprenaline was one of the first synthetic sympathomimetic amines, was the first selective β-adrenergic receptor agonist, and was the first major sympathomimetic agent devoid of pressor effects.[7][14]
Between 1963 and 1968 in England, Wales, Scotland, Ireland, Australia, and New Zealand there was an increase in deaths among people using isoprenaline to treat asthma. This was attributed to unintentional overdose: the inhalers produced in that area were dispensing five times the dosage dispensed by inhalers produced in the United States and Canada, where the deaths were not observed.[38][39]
The short duration of action and poor oral activity of isoprenaline led to the development of the much longer-acting and orally active orciprenaline (metaproterenol).[40][7]
Society and culture
[edit]Names
[edit]Isoprenaline is the major generic name of the drug and its INN, BAN, and DCF.[35][1][36][2] Isoprenalina is its Italian generic name and its DCIT.[1][2] Isoprenaline hydrochloride and isoprenaline sulfate are its BANM in the case of the hydrochloride and sulfate salts, respectively.[1] Isoproterenol is another important synonym of the drug.[35][1][2] Isoproterenol hydrochloride is its USAN and JAN in the case of the hydrochloride salt and isoproterenol sulfate is its USAN and JAN in the case of the sulfate salt.[35][1][36][2] Other synonyms of the drug include isopropylnorepinephrine, isopropylnoradrenaline, and isopropydine.[35][1][36][2] It is additionally known by the former developmental code name WIN-5162.[1][2]
Isoprenaline has been marketed under many brand names worldwide.[1][2] These include Aleudrina, Asthpul, Iludrin, Iprenol, Isomenyl, Isuprel, Isoprenaline, Isoprenalina, Isoproterenol, Neo-Epinine, Neodrenal, Proternol, and Saventrine, among others.[1][2] It is also marketed as a combination drug with cromoglicic acid as Frenal Compositum, in combination with pronase as Isopal P, and in combination with atropine as Stmerin D.[2]
References
[edit]- ^ a b c d e f g h i j k l m Schweizerischer Apotheker-Verein (2004). Index Nominum: International Drug Directory. Index Nominum: International Drug Directory. Medpharm Scientific Publishers. p. 662. ISBN 978-3-88763-101-7. Retrieved 1 August 2024.
- ^ a b c d e f g h i j k "Isoprenaline". drugs.com. 6 August 2017. Archived from the original on 26 June 2019. Retrieved 1 August 2024.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y "Isoprenaline: Uses, Interactions, Mechanism of Action". DrugBank Online. 19 February 1948. Retrieved 31 July 2024.
- ^ a b c d e "Drugs@FDA: FDA-Approved Drugs". accessdata.fda.gov. Retrieved 31 July 2024.
- ^ a b c d e Waldeck B (June 2002). "Beta-adrenoceptor agonists and asthma--100 years of development". Eur J Pharmacol. 445 (1–2): 1–12. doi:10.1016/s0014-2999(02)01728-4. PMID 12065188.
- ^ a b c d e f Conolly ME, Davies DS, Dollery CT, Morgan CD, Paterson JW, Sandler M (November 1972). "Metabolism of isoprenaline in dog and man". Br J Pharmacol. 46 (3): 458–472. doi:10.1111/j.1476-5381.1972.tb08143.x. PMC 1666503. PMID 4656607.
- ^ a b c d e f g h i j k l m Morgan DJ (April 1990). "Clinical pharmacokinetics of beta-agonists". Clin Pharmacokinet. 18 (4): 270–294. doi:10.2165/00003088-199018040-00002. PMID 1969785.
- ^ a b c d Sterling LP (May 1995). "Beta adrenergic agonists". AACN Clin Issues. 6 (2): 271–278. doi:10.1097/00044067-199505000-00010. PMID 7743429.
- ^ a b c d e f g h i j "Label: Isoproterenol hydrochloride injection, solution". NIH DailyMed. September 10, 2013. Retrieved June 21, 2017.
- ^ Motwani SK, Saunders H (2024). "Inotropes". Anaesthesia & Intensive Care Medicine. 25 (3): 185–191. doi:10.1016/j.mpaic.2023.11.019.
- ^ a b c d e f "Isoproterenol". PubChem. Retrieved 31 July 2024.
- ^ a b c d e "Isoprenaline". ChemSpider. 21 July 2022. Retrieved 31 July 2024.
- ^ a b Konzett H (1981). "On the discovery of isoprenaline". Trends in Pharmacological Sciences. 2: 47–49. doi:10.1016/0165-6147(81)90259-5.
- ^ a b Ružena Č, Jindra V, Renáta H (18 June 2020). "Chirality of β2-agonists. An overview of pharmacological activity, stereoselective analysis, and synthesis". Open Chemistry. 18 (1): 628–647. doi:10.1515/chem-2020-0056. ISSN 2391-5420.
- ^ a b c d e Mozayani A, Raymon L (2003). Handbook of Drug Interactions: A Clinical and Forensic Guide. Springer Science & Business Media. pp. 541–542. ISBN 978-1-59259-654-6.
- ^ Cohagan B, Brandis D (August 2022). "Torsade de Pointes". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 29083738. NBK459388.
- ^ Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, et al. (August 2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society". Circulation. 140 (8): e382–e482. doi:10.1161/CIR.0000000000000628. PMID 30586772.
- ^ National Asthma Education and Prevention Program Expert Panel (August 28, 2007). "Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma" (PDF). NIH National Heart, Lung, and Blood Institute.
- ^ Jongman JK, Jepkes-Bruin N, Ramdat Misier AR, Beukema WP, Delnoy PP, Oude Lutttikhuis H, et al. (April 2007). "Electrical storms in Brugada syndrome successfully treated with isoproterenol infusion and quinidine orally". Netherlands Heart Journal. 15 (4): 151–155. doi:10.1007/BF03085972. PMC 1847769. PMID 17612676.
- ^ Hoff R, Koh CK (2018). "Isoproterenol Induced Insulin Resistance Leading to Diabetic Ketoacidosis in Type 1 Diabetes Mellitus". Case Reports in Endocrinology. 2018: 4328954. doi:10.1155/2018/4328954. PMC 6311779. PMID 30647979.
- ^ a b Emilien G, Maloteaux JM (February 1998). "Current therapeutic uses and potential of beta-adrenoceptor agonists and antagonists". Eur J Clin Pharmacol. 53 (6): 389–404. doi:10.1007/s002280050399. PMID 9551698.
- ^ Furchgott RF, Bhadrakom S (June 1953). "Reactions of strips of rabbit aorta to epinephrine, isopropylarterenol, sodium nitrite and other drugs". The Journal of Pharmacology and Experimental Therapeutics. 108 (2): 129–143. PMID 13062084.
- ^ Copik AJ, Baldys A, Nguyen K, Sahdeo S, Ho H, Kosaka A, et al. (21 January 2015). "Isoproterenol acts as a biased agonist of the alpha-1A-adrenoceptor that selectively activates the MAPK/ERK pathway". PLOS ONE. 10 (1): e0115701. Bibcode:2015PLoSO..1015701C. doi:10.1371/journal.pone.0115701. PMC 4301629. PMID 25606852.
- ^ Kleinau G, Pratzka J, Nürnberg D, Grüters A, Führer-Sakel D, Krude H, et al. (October 2011). "Differential modulation of Beta-adrenergic receptor signaling by trace amine-associated receptor 1 agonists". PLOS ONE. 6 (10): e27073. Bibcode:2011PLoSO...627073K. doi:10.1371/journal.pone.0027073. PMC 3205048. PMID 22073124.
Table 1. EC50 values of different agonists at hTAAR1, hADRB1 and hADRB2
- ^ Korbut R (2017). Farmakologia (in Polish). Wydawnictwo Lekarskie PZWL. p. 36. ISBN 978-83-200-5368-5.
- ^ a b Mehta A (January 27, 2011). "Notes - Medicinal Chemistry of the Peripheral Nervous System - Adrenergics and Cholinergic". Pharmaxchange. Archived from the original on 4 November 2010. Retrieved June 21, 2017.
- ^ a b George CF (1981). "Drug metabolism by the gastrointestinal mucosa". Clin Pharmacokinet. 6 (4): 259–274. doi:10.2165/00003088-198106040-00002. PMID 6113909.
- ^ Redwood D (January 1969). "Conservative treatment of chronic heart block". Br Med J. 1 (5635): 26–29. doi:10.1136/bmj.1.5635.26. PMC 1981820. PMID 5761891.
- ^ a b c d Olesen J, Hougård K, Hertz M (1978). "Isoproterenol and propranolol: ability to cross the blood-brain barrier and effects on cerebral circulation in man". Stroke. 9 (4): 344–349. doi:10.1161/01.str.9.4.344. PMID 209581.
Mean extraction of isoproterenol in a single passage of the brain circulation was 3.8% and the calculated PS product was 2.0 ml/100g/min. The mean extraction of propranolol was 63.0% and the mean PS product 46.7 ml/100 g/min. [...] Passage of Isoproterenol and Propranolol Across Blood–Brain Barrier: No data are available in the literature concerning the ability of isoproterenol to cross the blood-brain barrier. From the hydrophilic nature of the molecule one might expect diffusion to be very slow, but the possibility of active uptake mechanisms still existed. The extraction of 3.8% found in the present study corresponds to that of sodium or other hydrophilic molecules.12 It is likely that a significant part of this extraction stems from areas known to be devoid of a blood-brain barrier. The extraction is clearly much smaller than that seen for amino acids and other substances that pass the barrier by facilitated diffusion.14
- ^ Crystal GJ, Salem MR (October 2002). "Beta-adrenergic stimulation restores oxygen extraction reserve during acute normovolemic hemodilution". Anesth Analg. 95 (4): 851–857, table of contents. doi:10.1097/00000539-200210000-00011. PMID 12351256.
The lack of effect of blood-borne catecholamines, including isoproterenol, on cerebral blood flow has been attributed to their inability to cross the blood-brain barrier (26).
- ^ a b Procaccini DE, Sawyer JE, Watt KM (2019). "Pharmacology of Cardiovascular Drugs". Critical Heart Disease in Infants and Children. pp. 192–212.e6. doi:10.1016/B978-1-4557-0760-7.00019-X. ISBN 978-1-4557-0760-7. S2CID 81053428.
- ^ a b Szymanski MW, Singh DP (2023). "Isoproterenol". StatPearls. StatPearls Publishing. PMID 30252298. NBK526042.
- ^ "Epinephrine". PubChem. Retrieved 1 August 2024.
- ^ "Norepinephrine". PubChem. Retrieved 1 August 2024.
- ^ a b c d e Elks J (2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer US. p. 710. ISBN 978-1-4757-2085-3. Retrieved 1 August 2024.
- ^ a b c d Morton IK, Hall JM (2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Netherlands. p. 157. ISBN 978-94-011-4439-1. Retrieved 1 August 2024.
- ^ Morton IK, Hall JM (2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Netherlands. p. 164. ISBN 978-94-011-4439-1. Retrieved 2024-08-01.
- ^ Pearce N, Hensley MJ (1998). "Epidemiologic studies of beta agonists and asthma deaths". Epidemiologic Reviews. 20 (2): 173–186. doi:10.1093/oxfordjournals.epirev.a017979. PMID 9919437.
- ^ Jalba MS (2008). "Three generations of ongoing controversies concerning the use of short acting beta-agonist therapy in asthma: a review". The Journal of Asthma. 45 (1): 9–18. doi:10.1080/02770900701495512. PMID 18259990. S2CID 31732029.
- ^ Dserendorf H (1995). Drug Actions: Basic Principles and Theraputic Aspects. CRC-Press. p. 227. ISBN 978-0-8493-7774-7. Retrieved 1 August 2024.